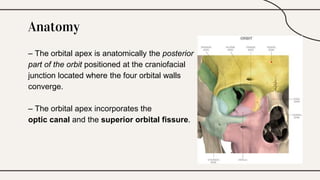
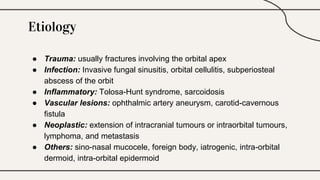
Orbital apex syndrome, also known as Jacod syndrome, involves a collection of cranial nerve deficits due to various pathologies affecting the orbital apex, impacting structures like the optic nerve and oculomotor nerve. Clinical signs include ophthalmoplegia, proptosis, and ipsilateral sensory deficits, with potential causes ranging from trauma to neoplastic growths. Management focuses on addressing the underlying cause, including options like observation, surgical intervention, and corticosteroids.