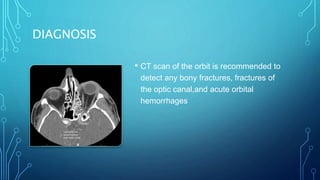
This document provides an overview of optic neuropathy, including its causes, clinical approach, and treatment. It discusses various types of optic neuropathy such as inflammatory optic neuritis, non-arteritic and arteritic anterior ischemic optic neuropathy, traumatic optic neuropathy, infiltrative optic neuropathy from tumors, compressive optic neuropathy from lesions, and hereditary and nutritional optic neuropathies. For each type, it describes the symptoms, signs, investigations, and management approach. The document is a comprehensive review of the etiology, diagnosis, and management of optic neuropathies.