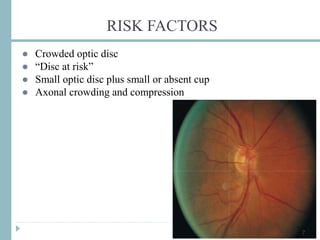
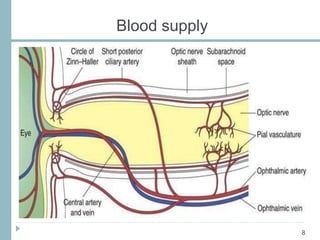
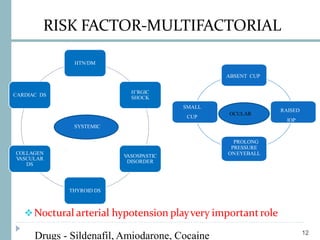
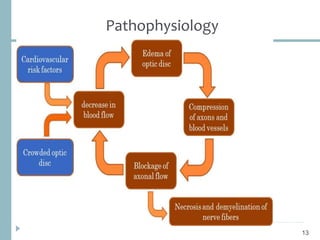
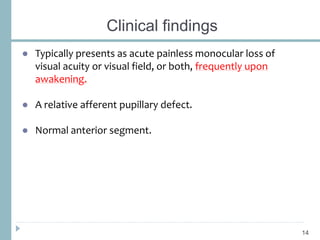
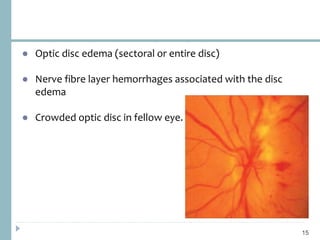
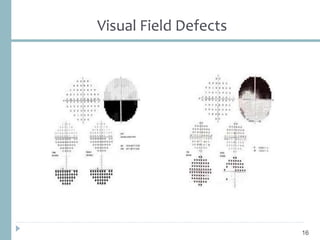
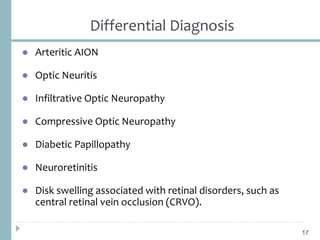
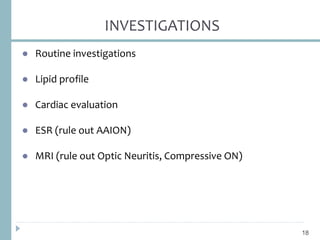
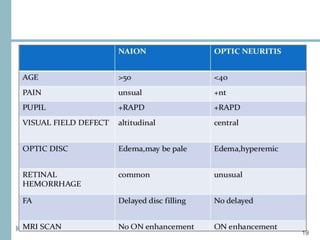
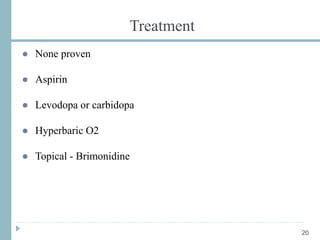
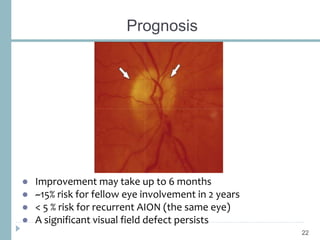
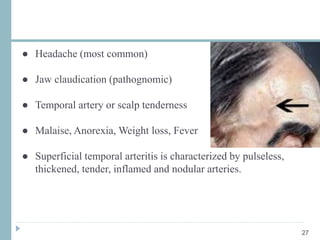
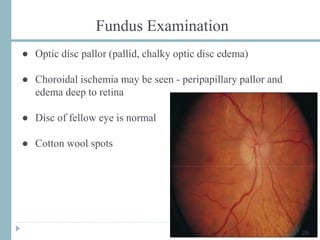
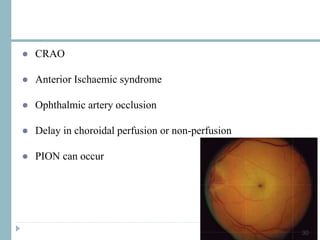
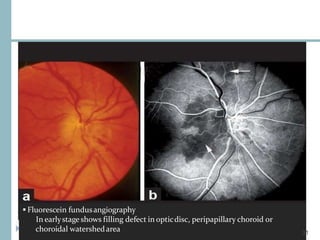
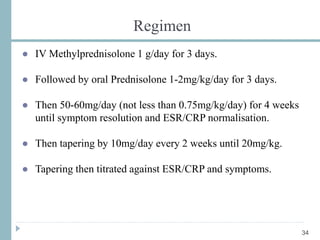
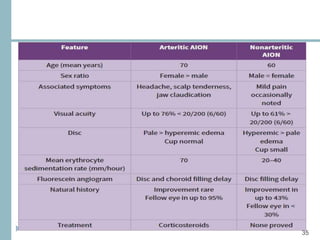
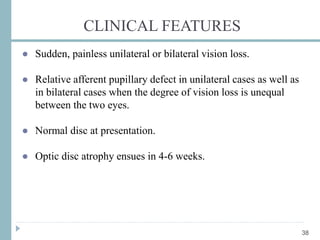
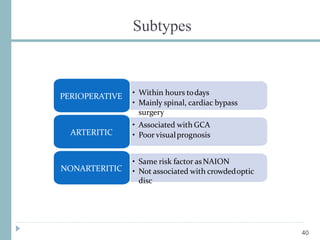
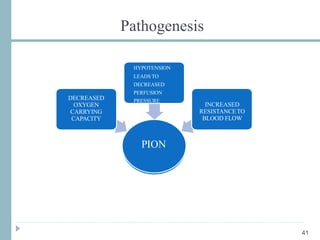
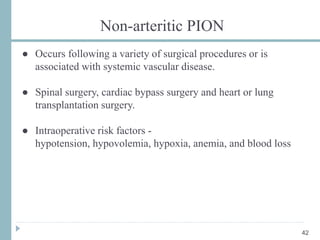
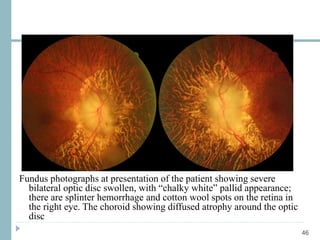
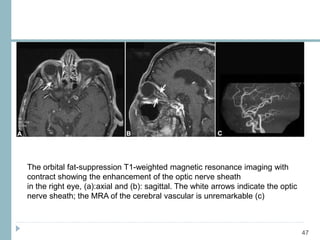
This document discusses different types of ischemic optic neuropathy including anterior ischemic optic neuropathy (AION), non-arteritic anterior ischemic optic neuropathy (NAION), arteritic anterior ischemic optic neuropathy (AAION), and posterior ischemic optic neuropathy (PION). NAION is the most common type, accounting for 90-95% of AION cases. AAION is caused by giant cell arteritis and results in more severe vision loss. Risk factors, clinical presentations, investigations, and treatments are described for each condition. A case report demonstrates the findings and management of a patient with AAION.