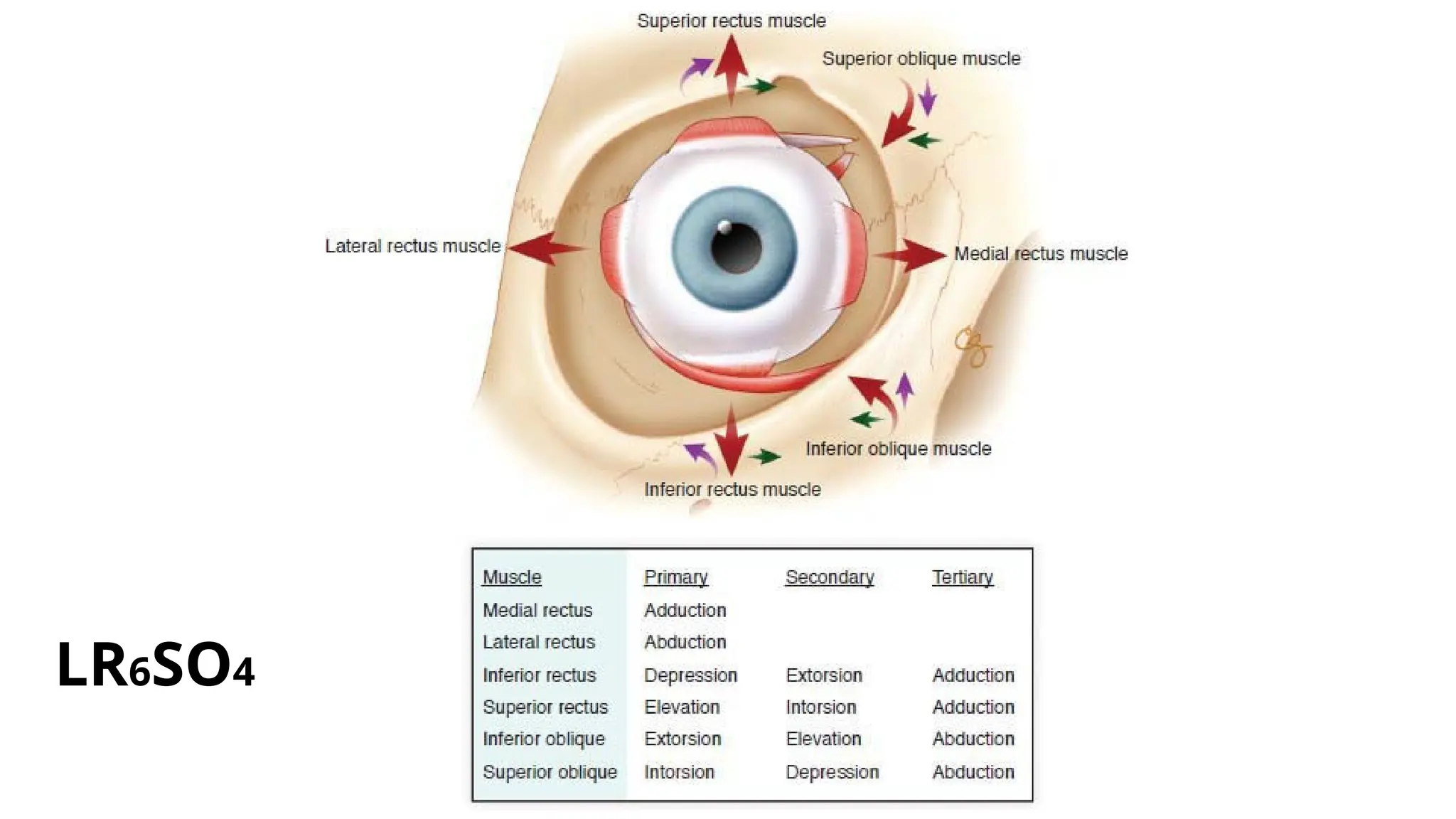
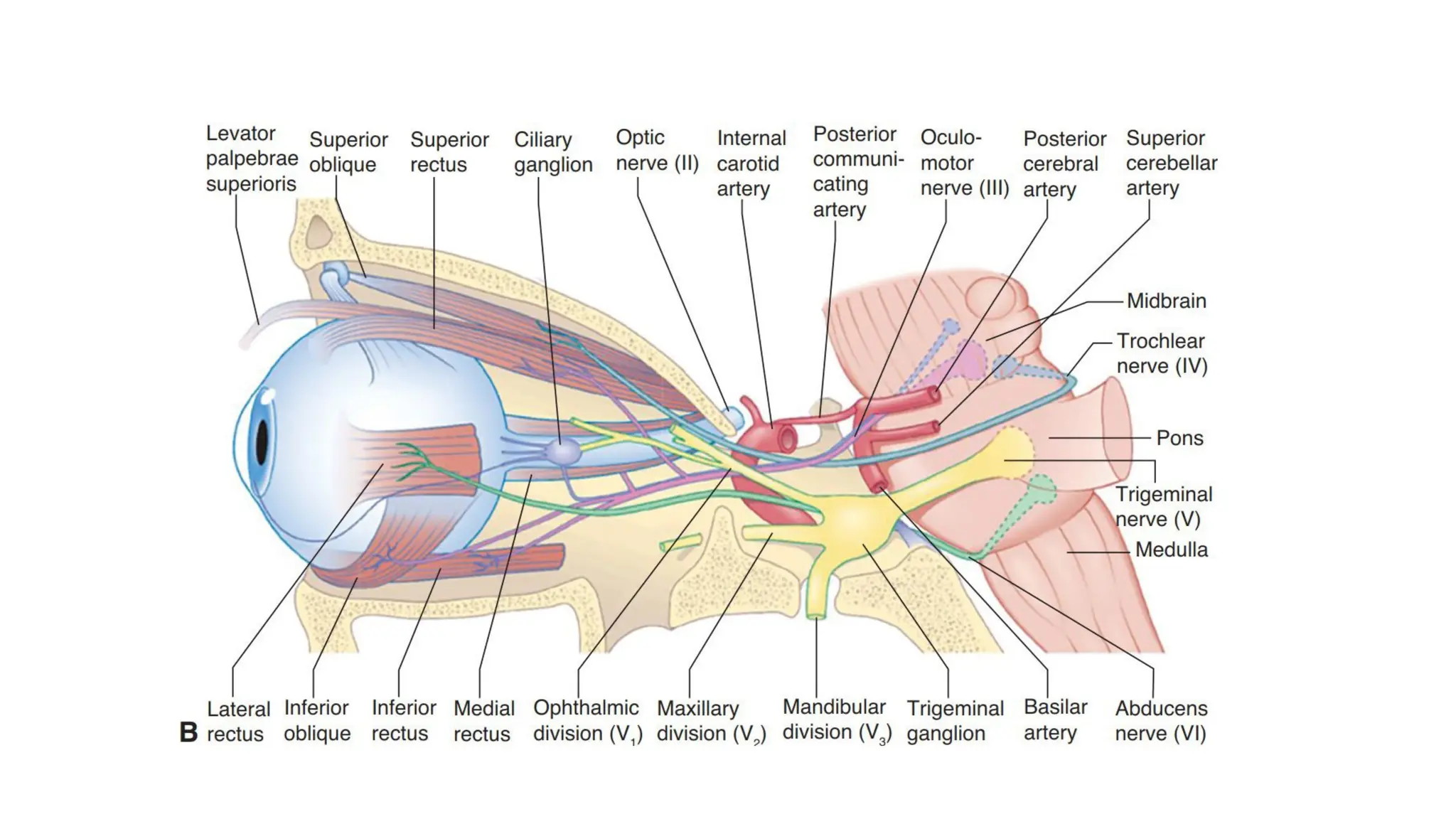
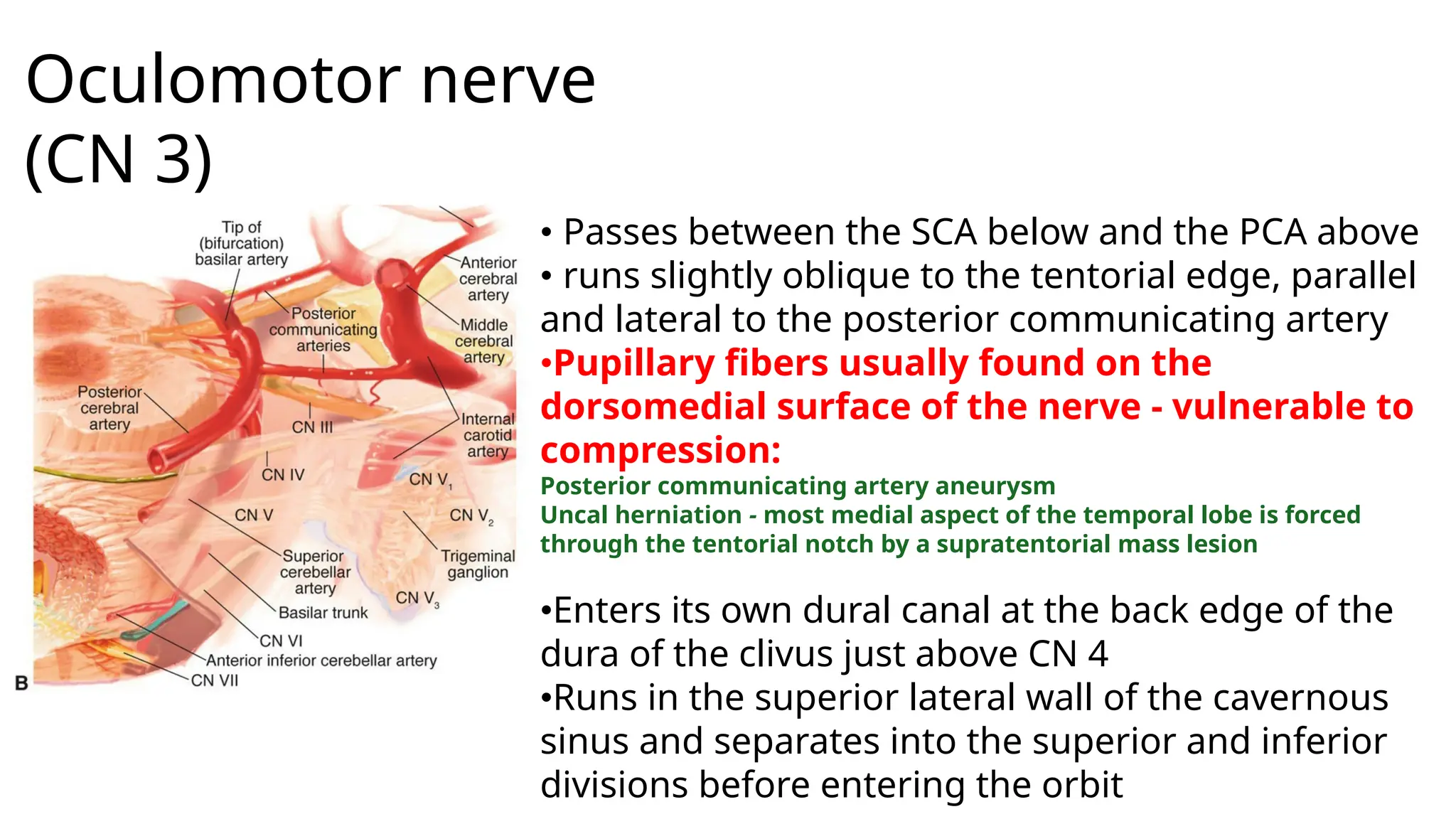
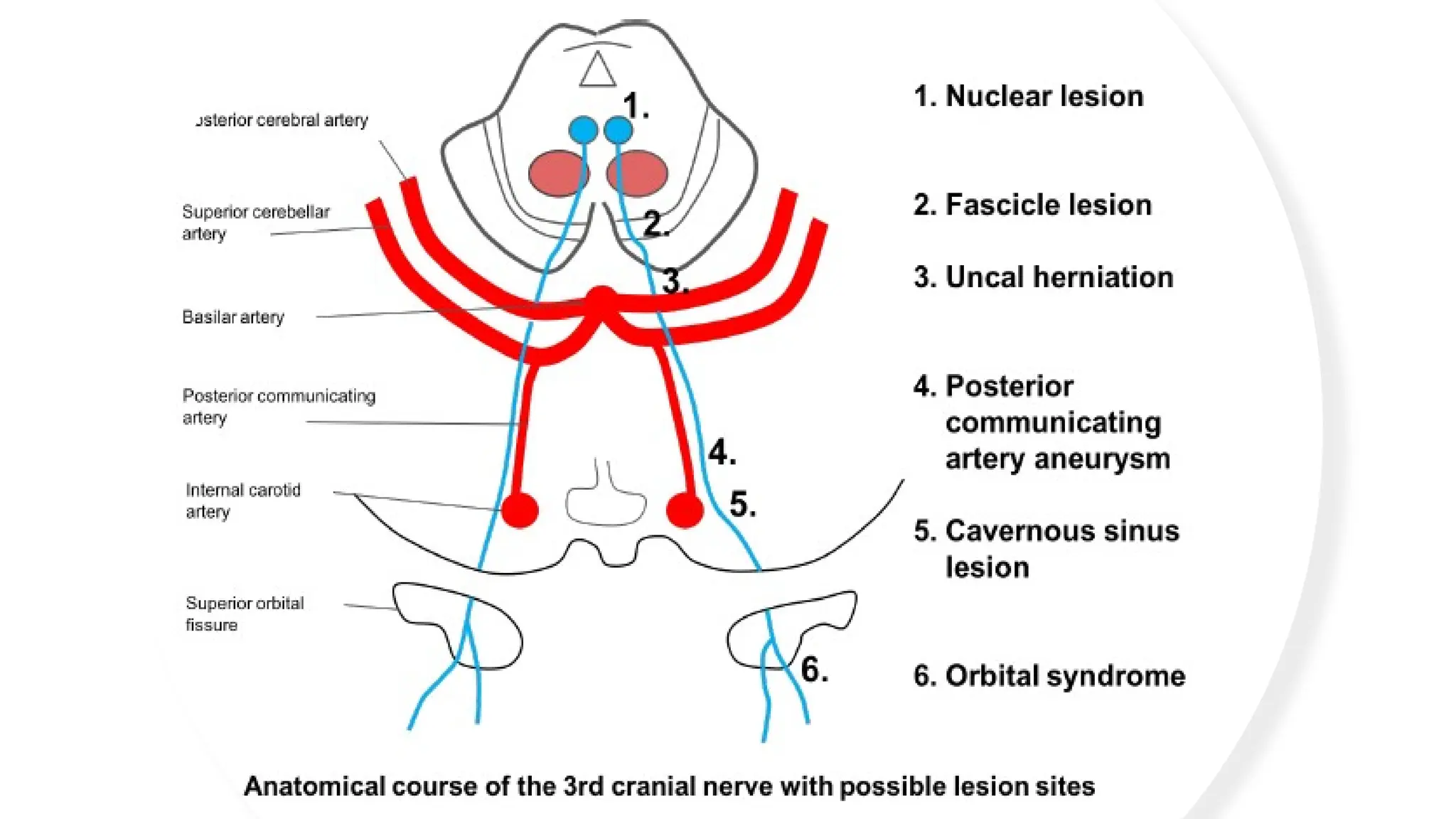
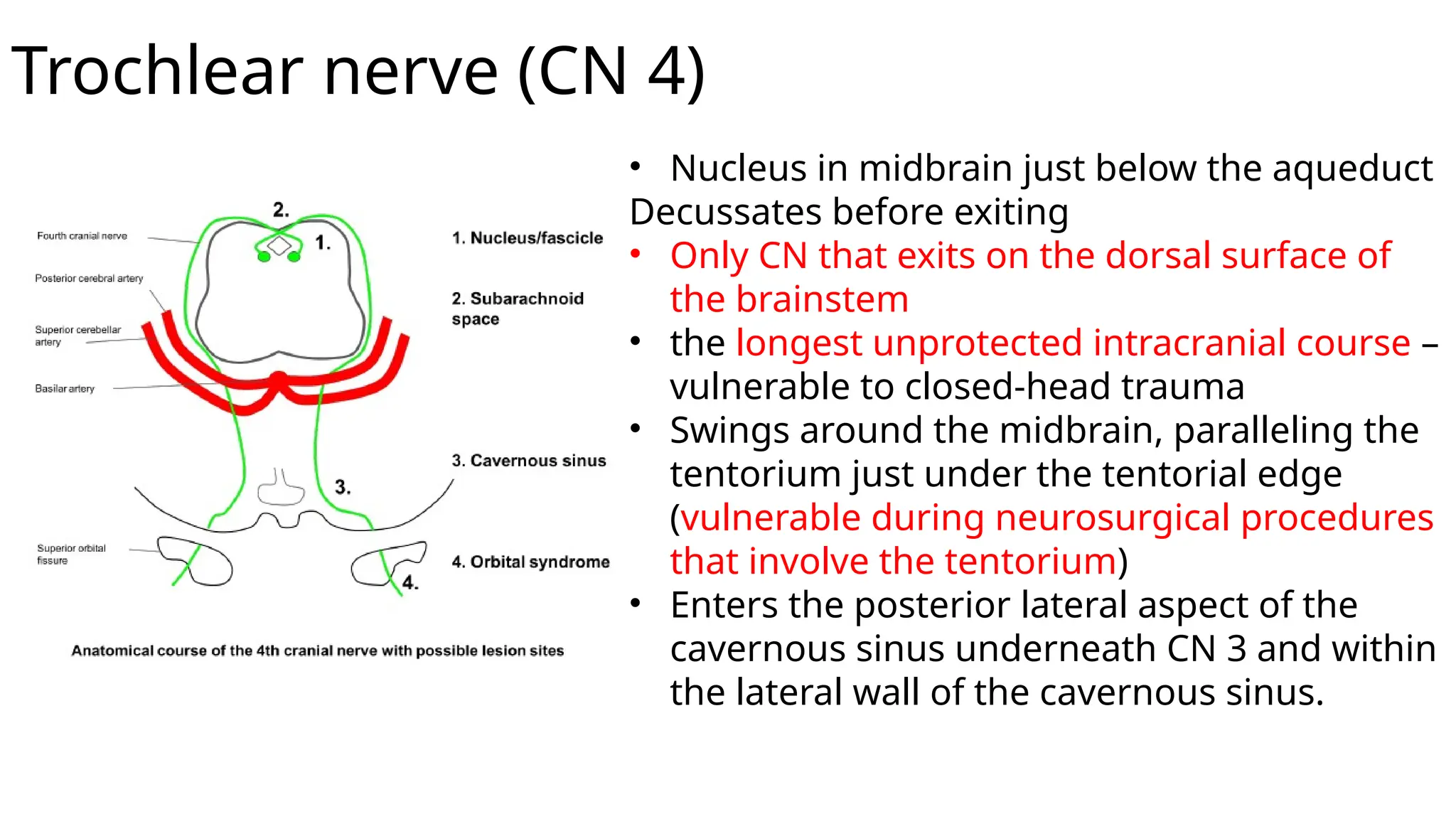
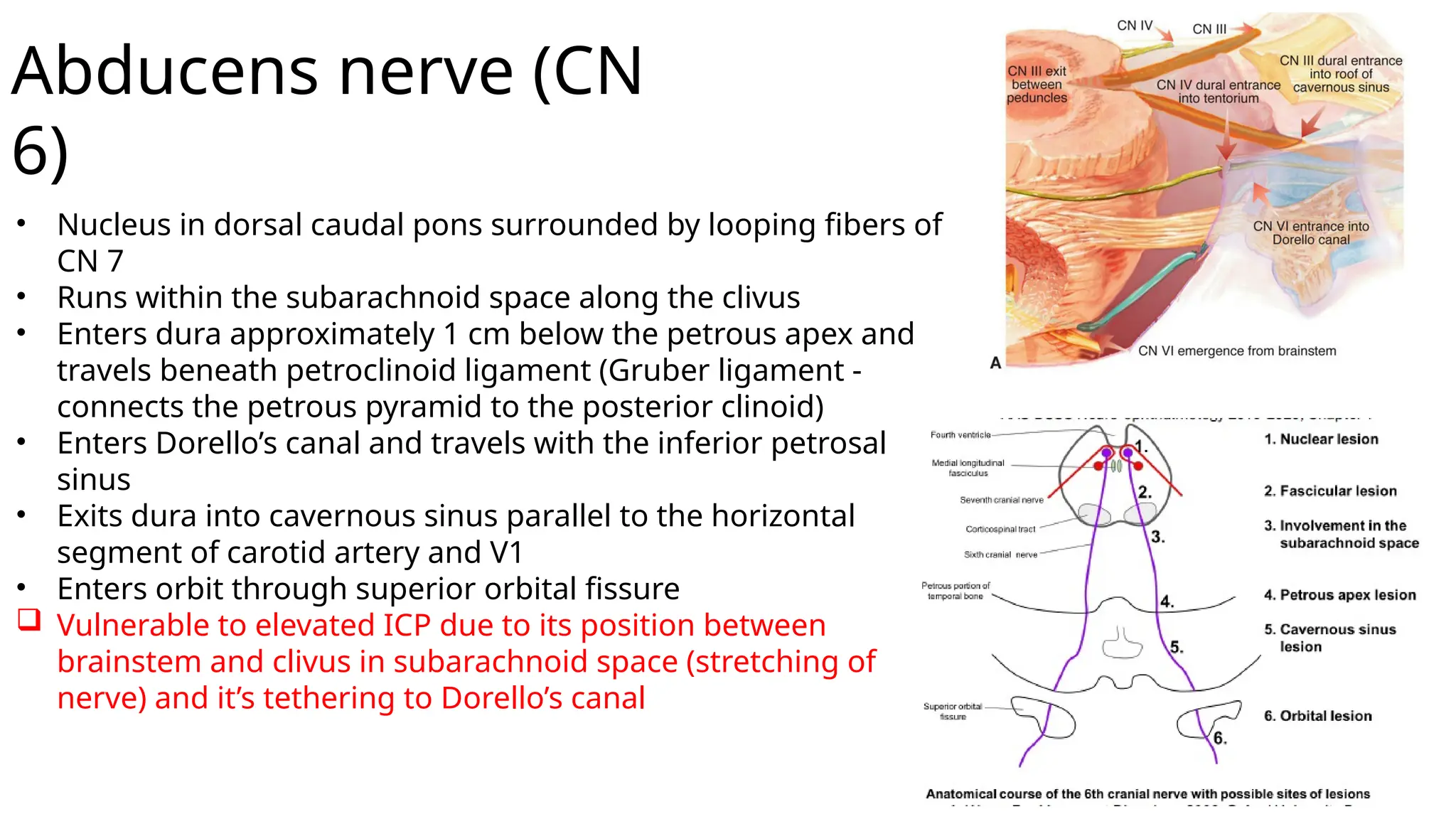
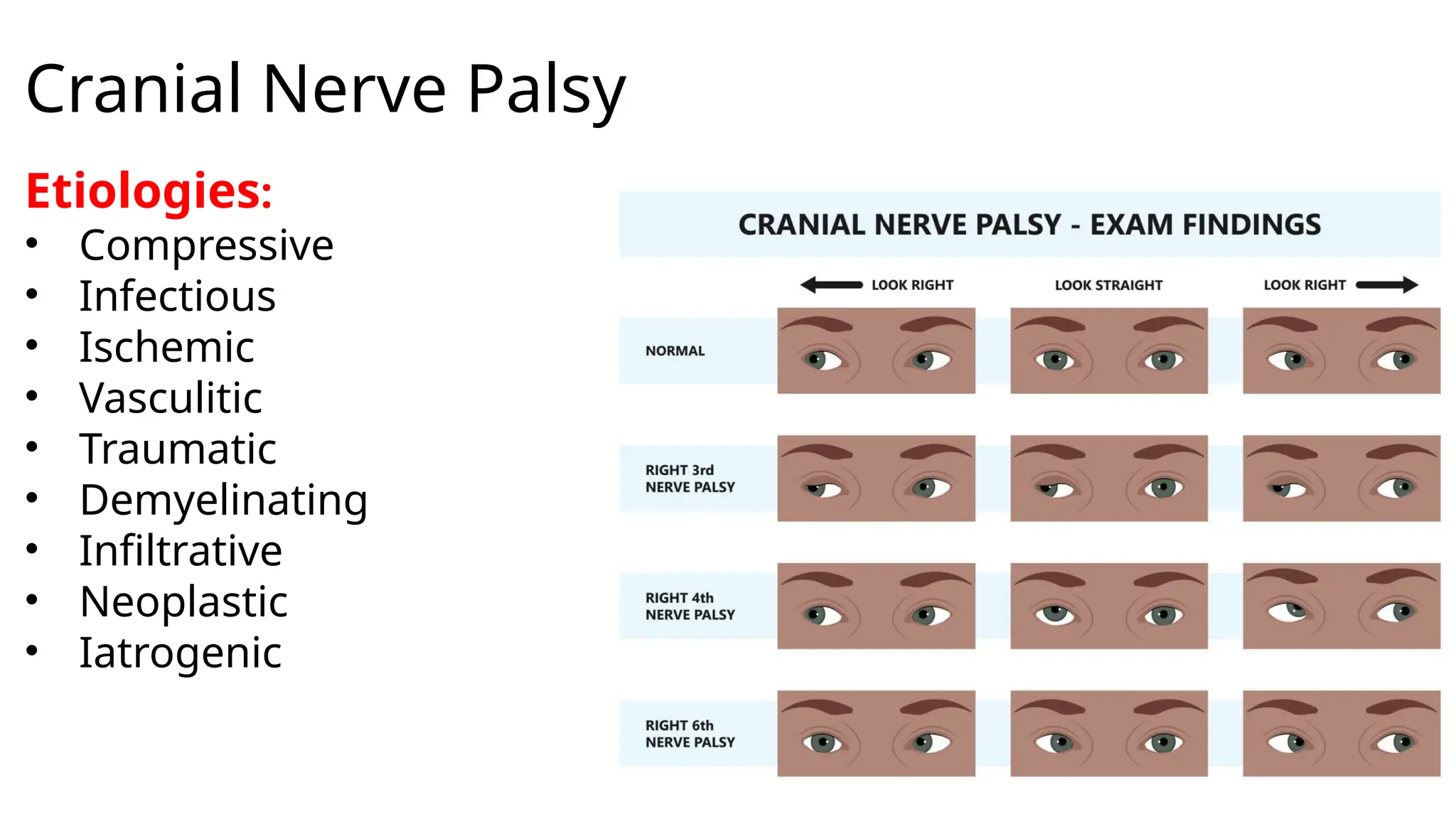
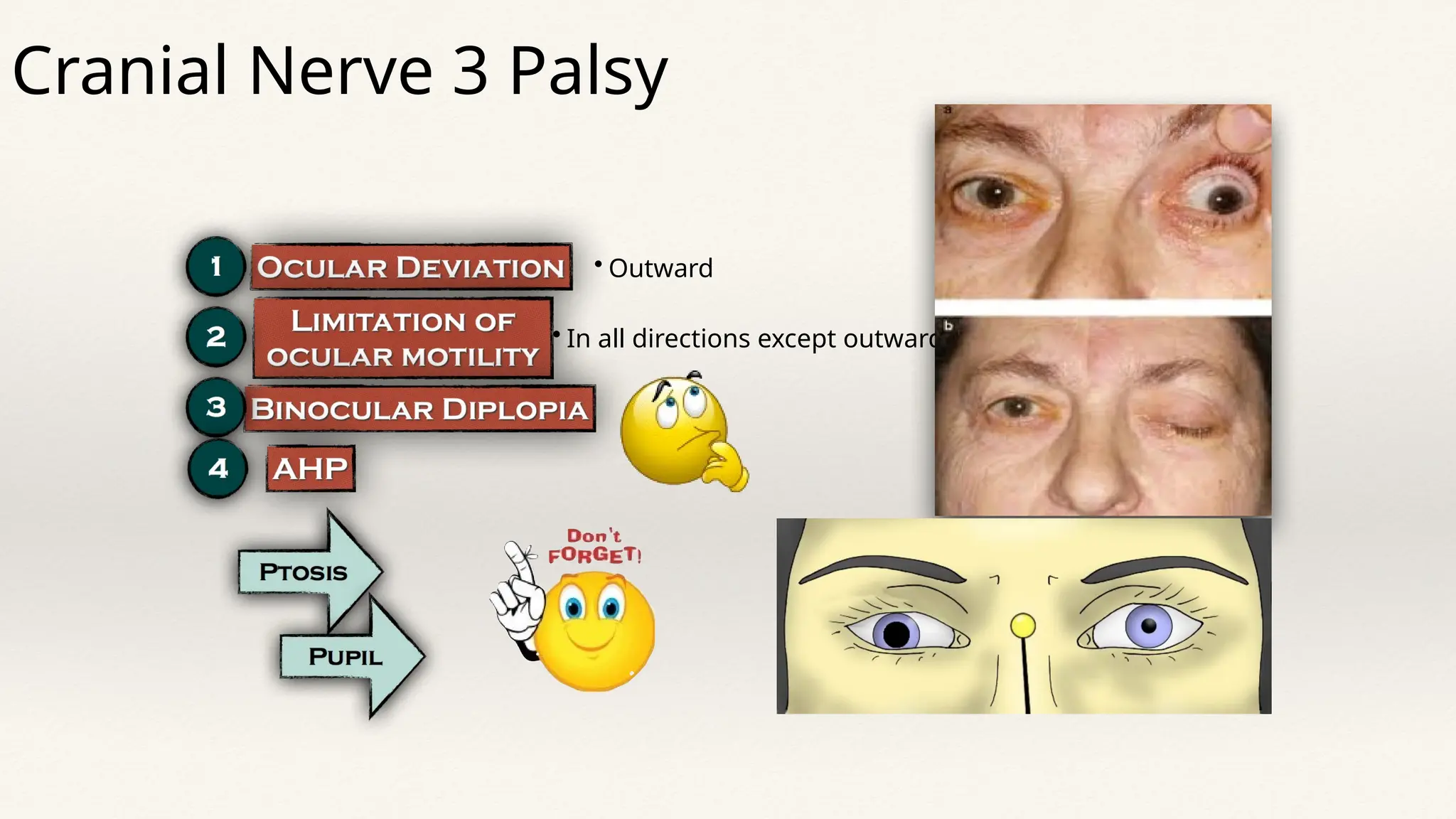
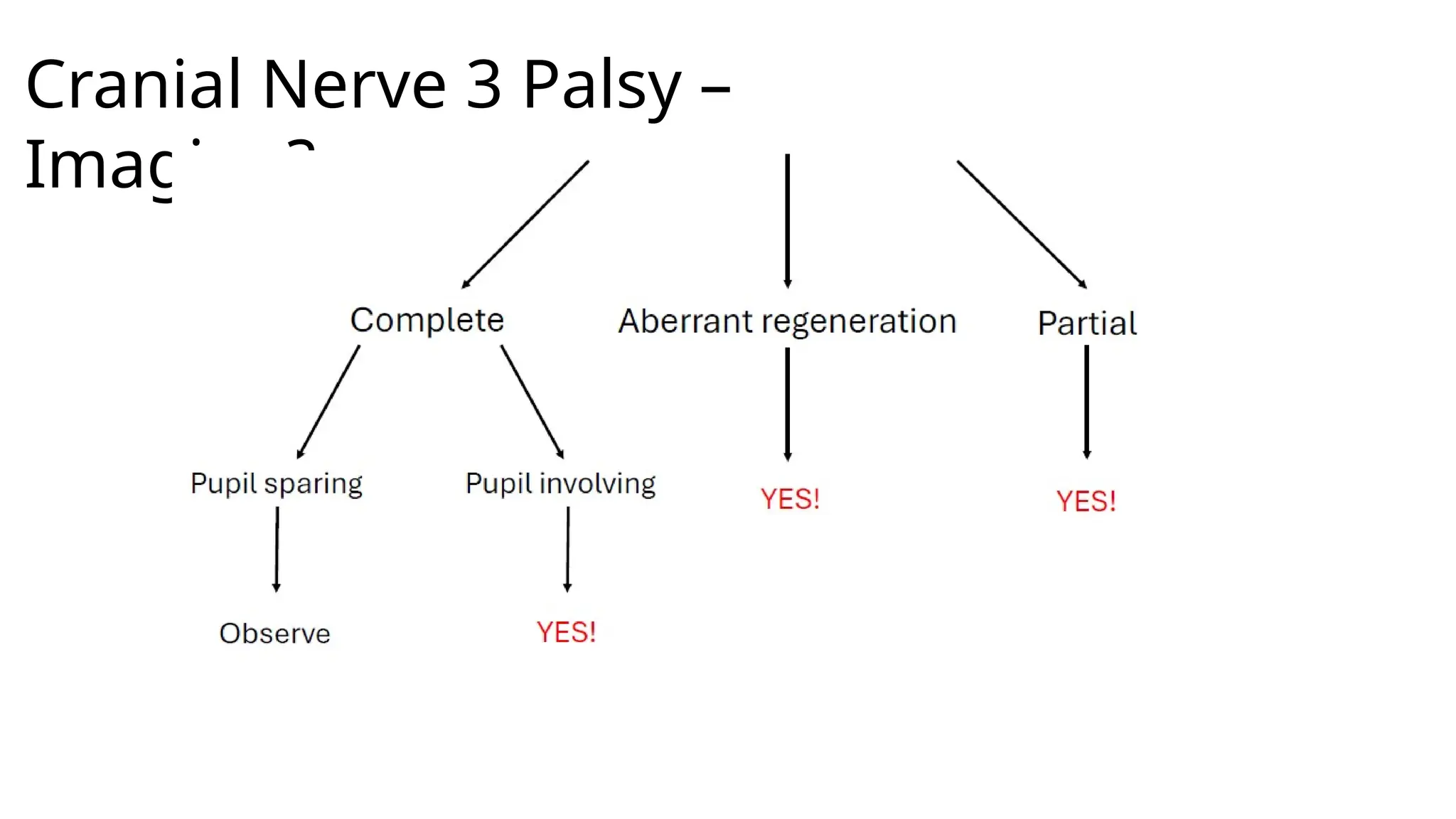
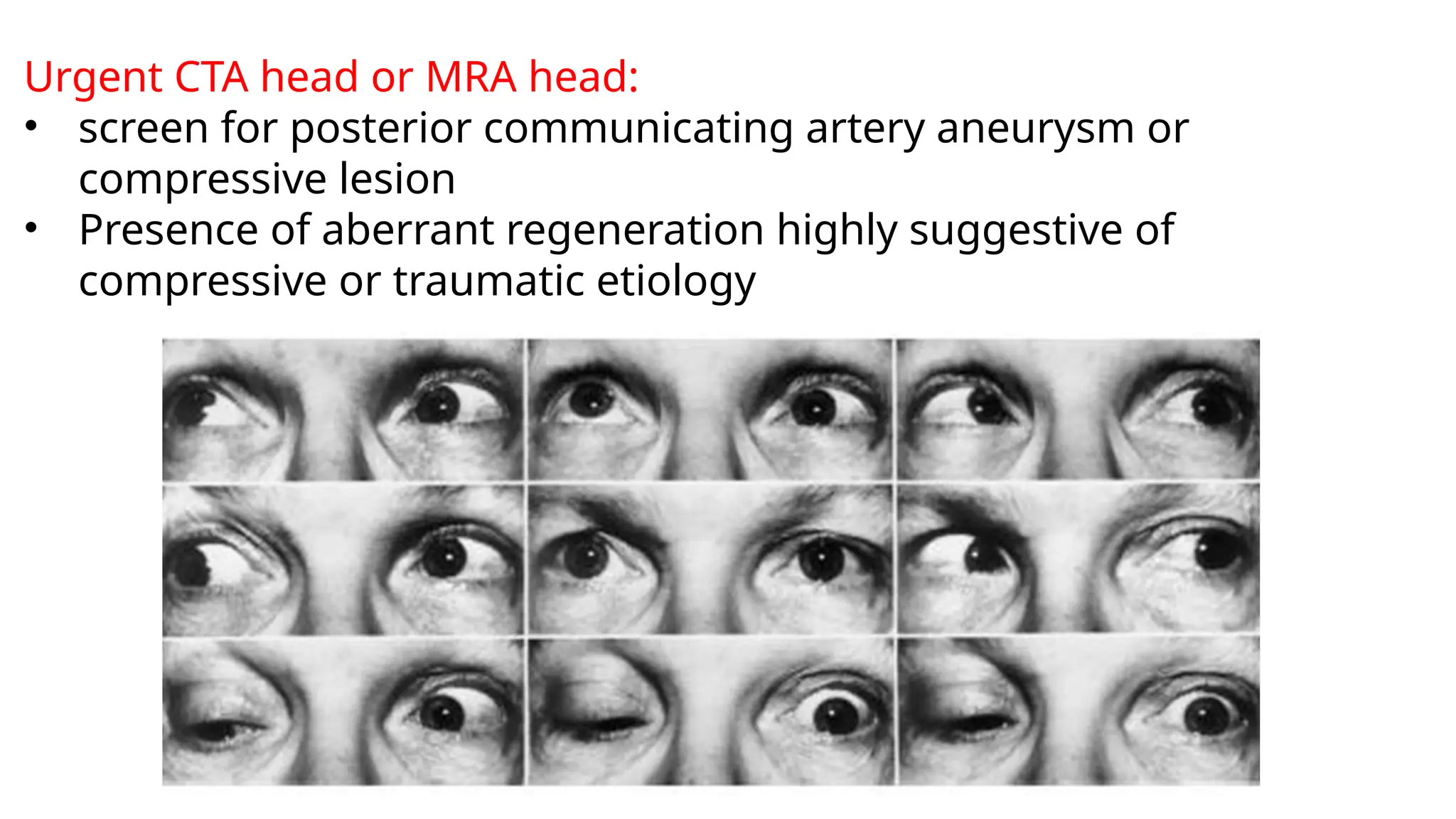
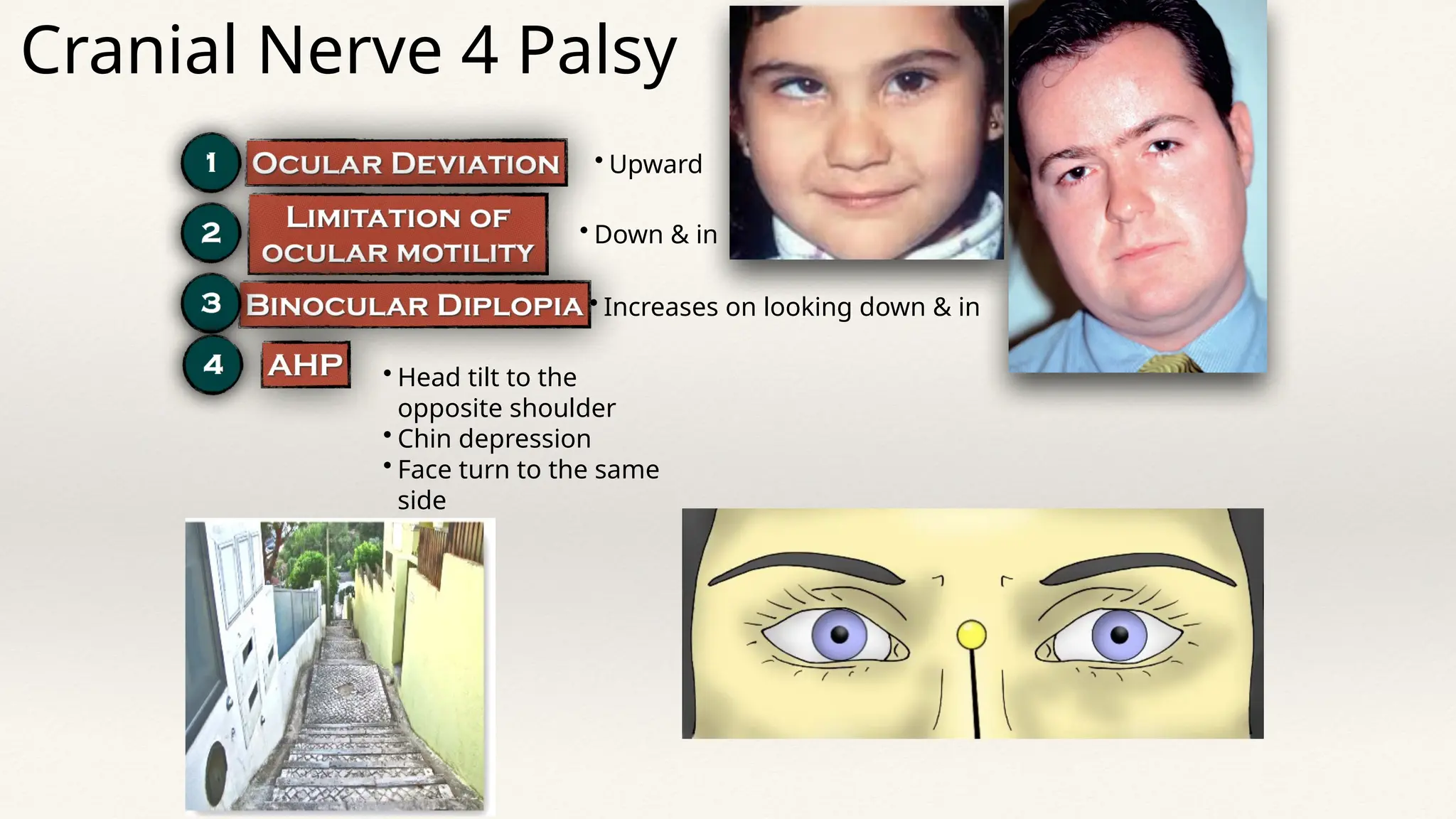
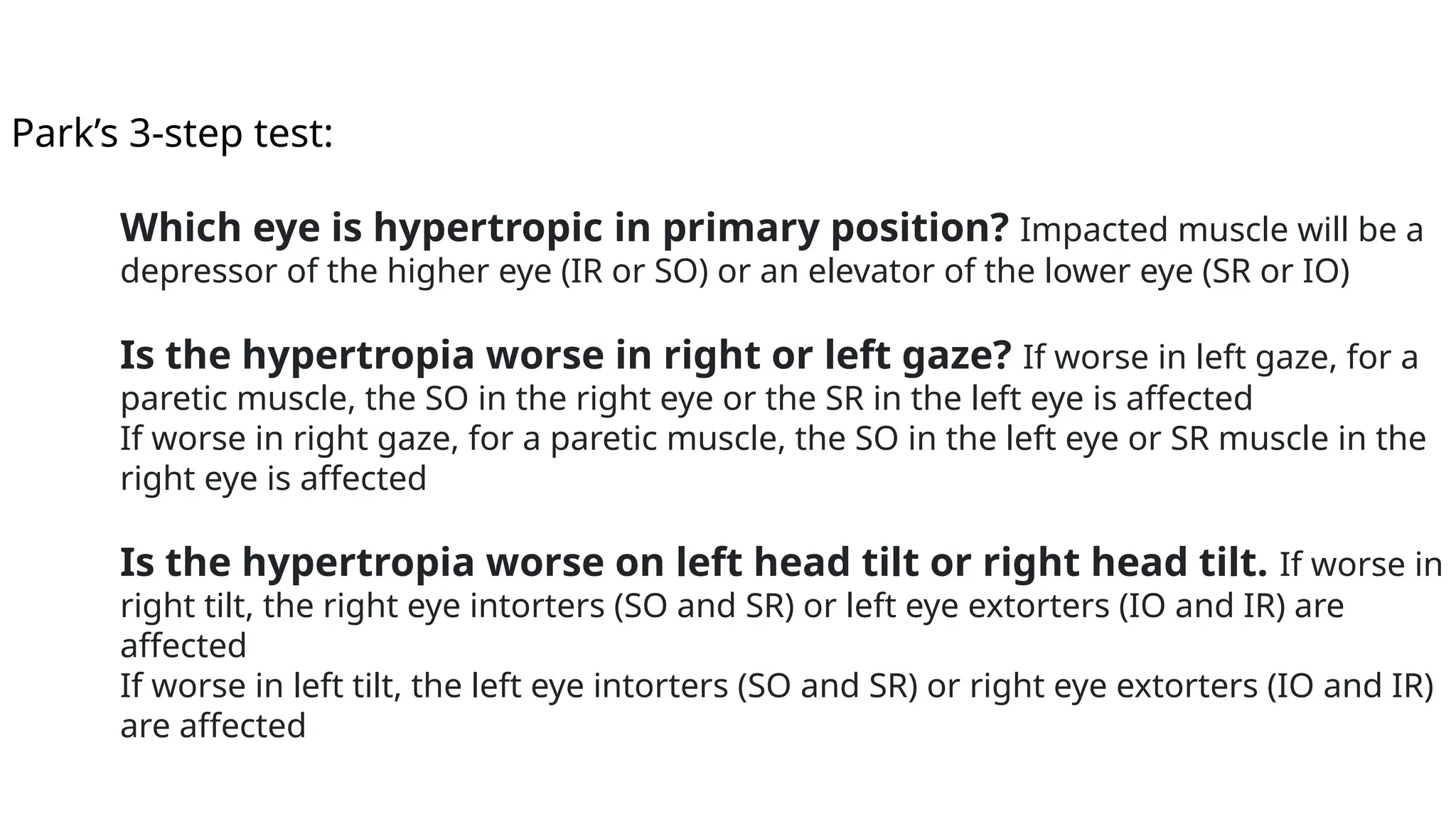
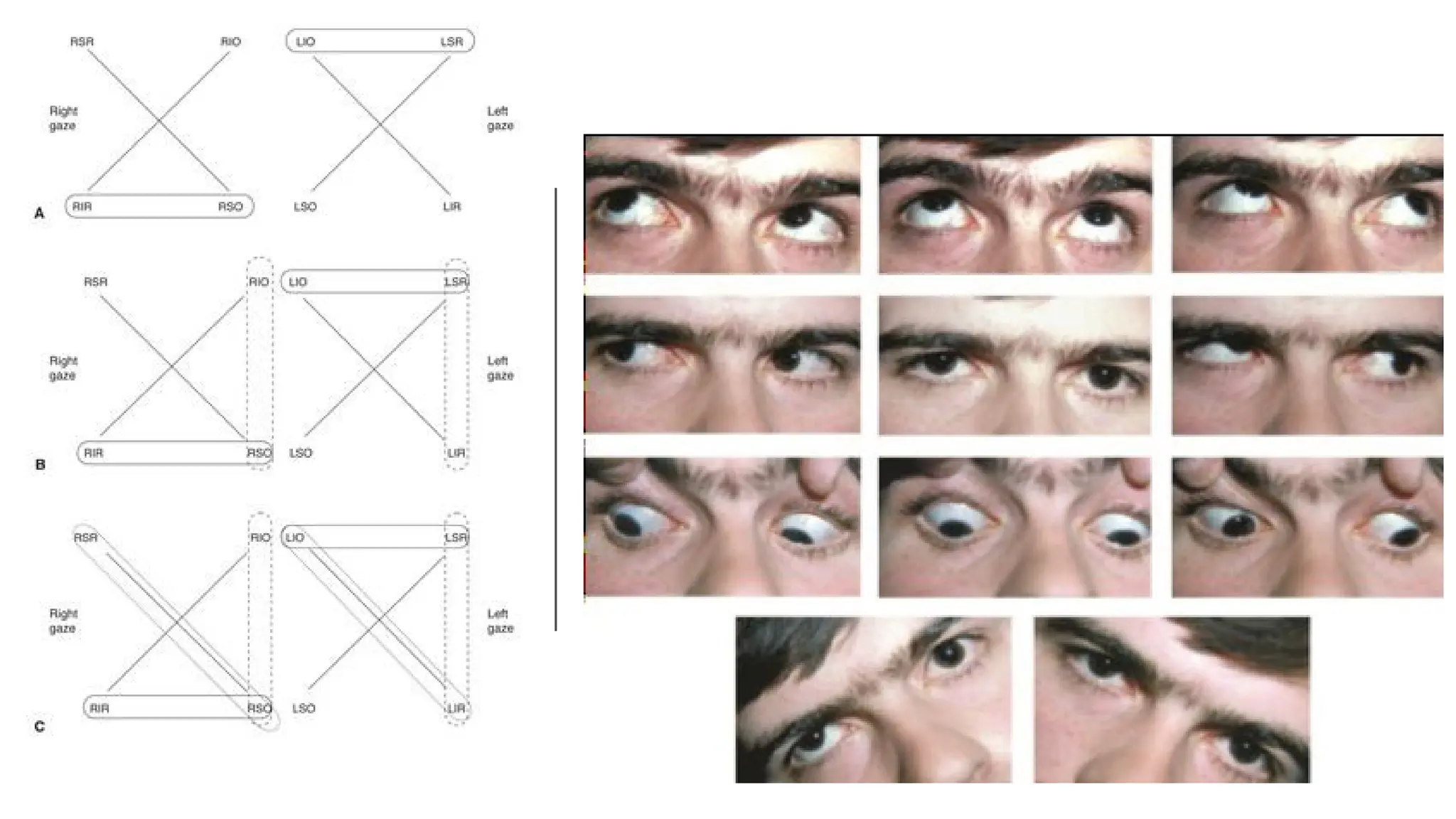
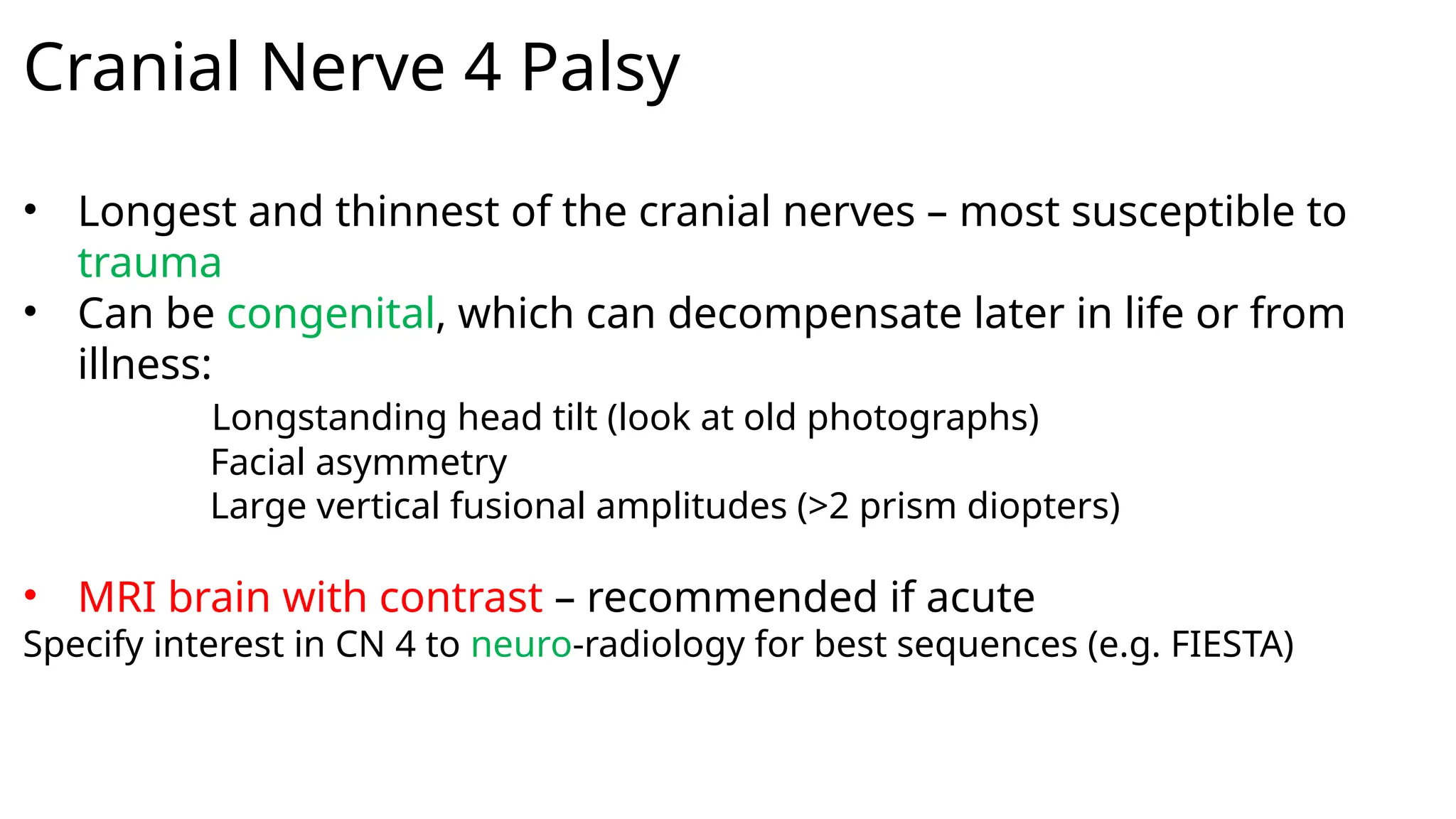
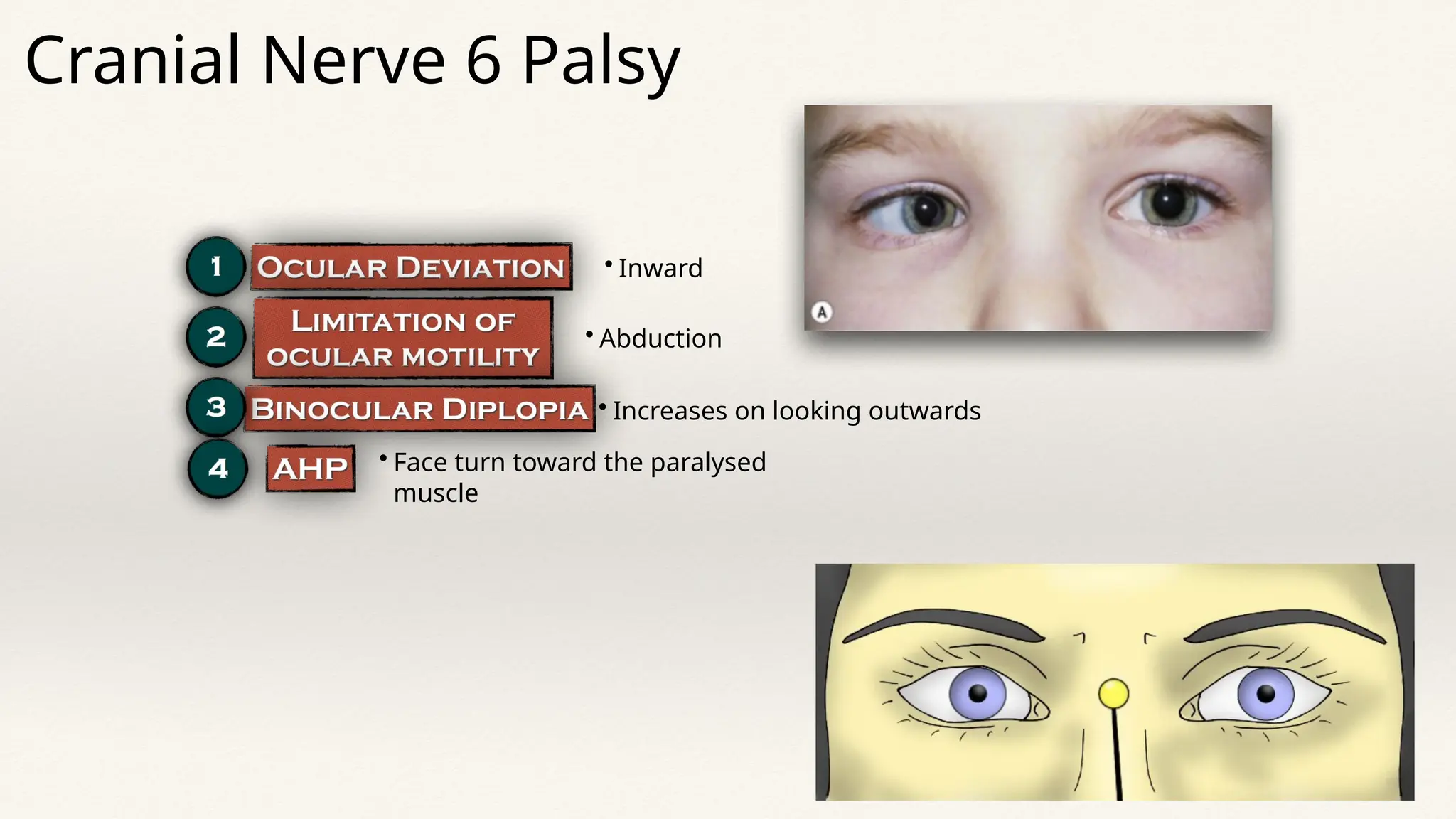
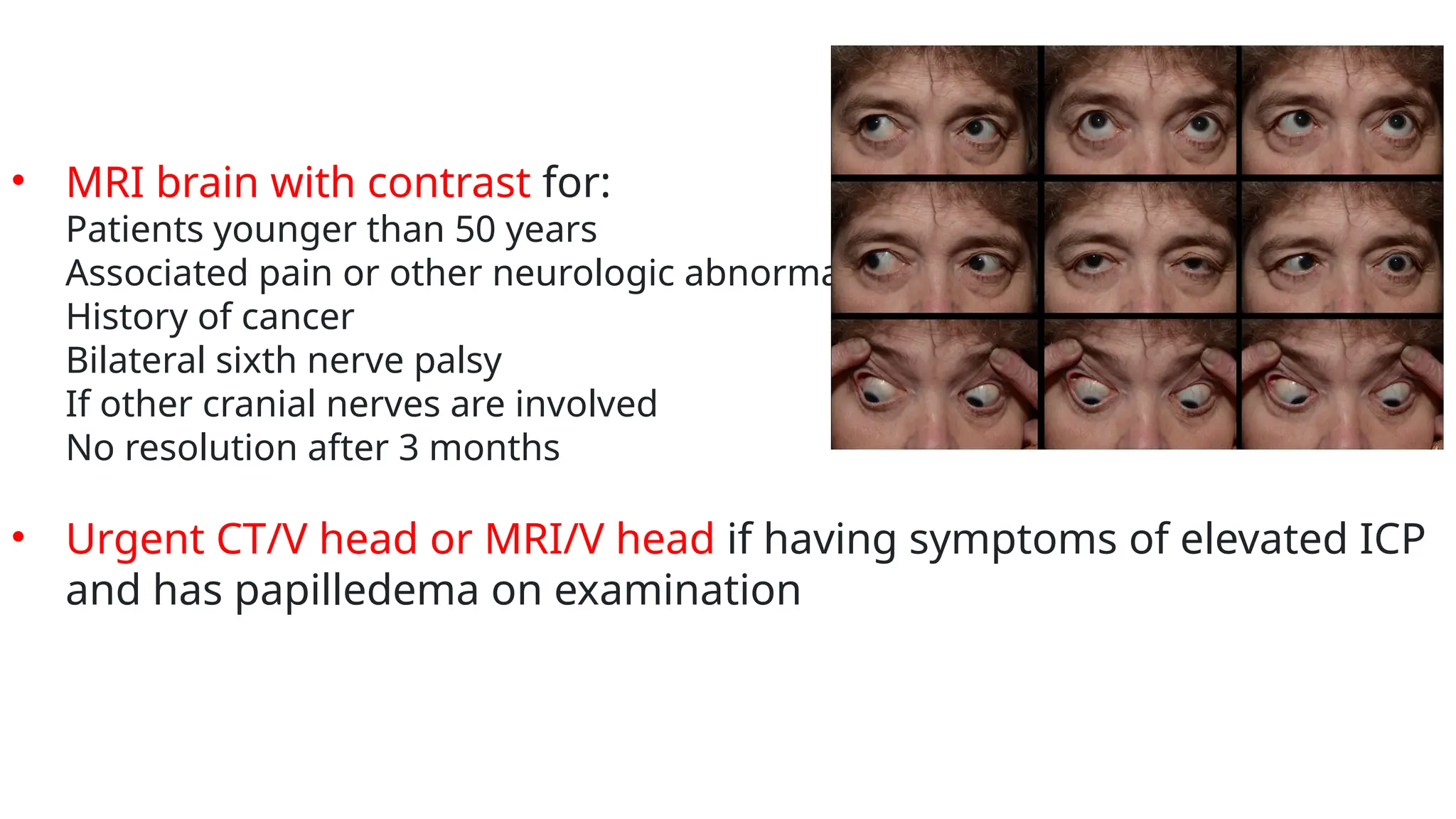
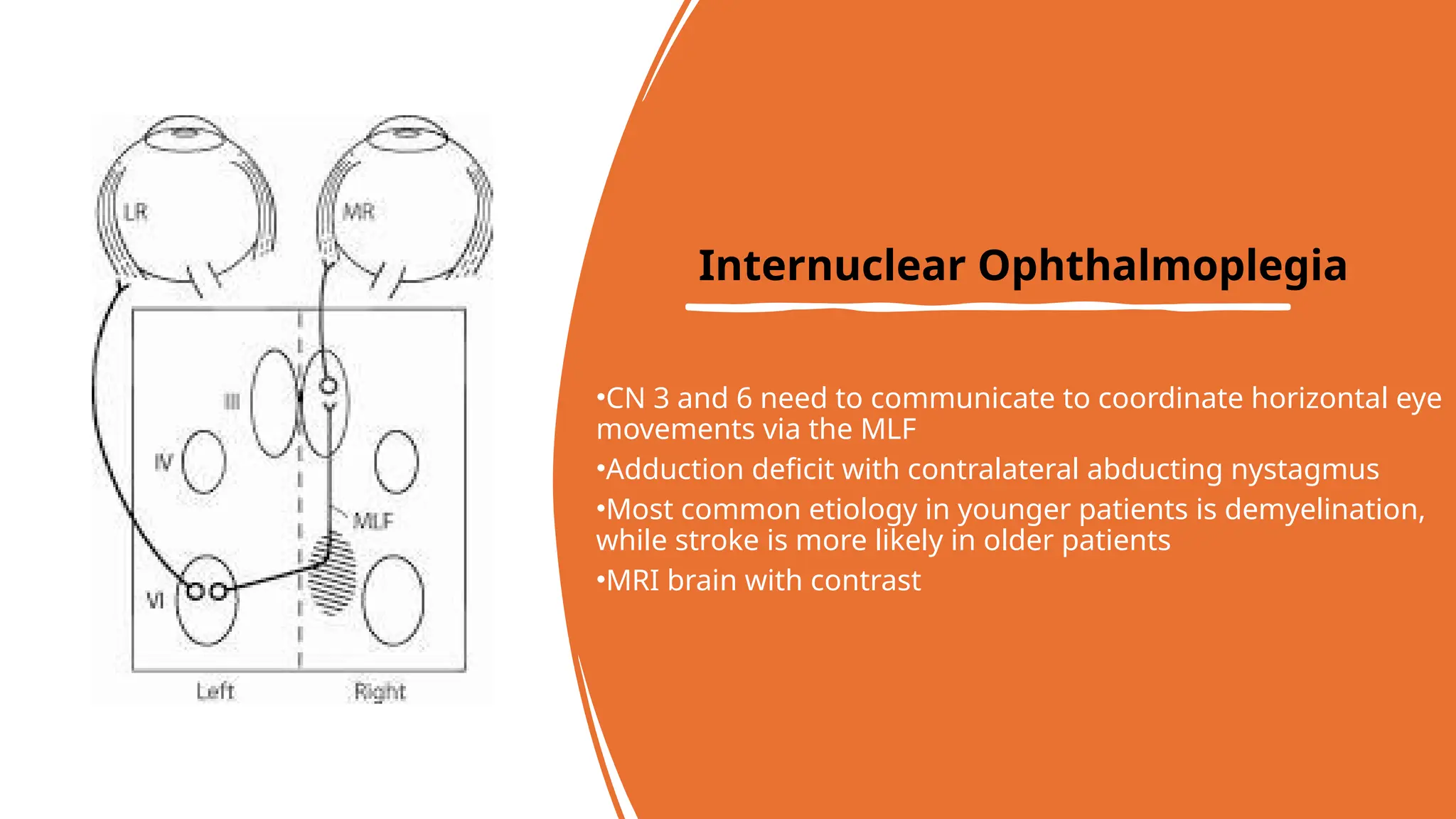
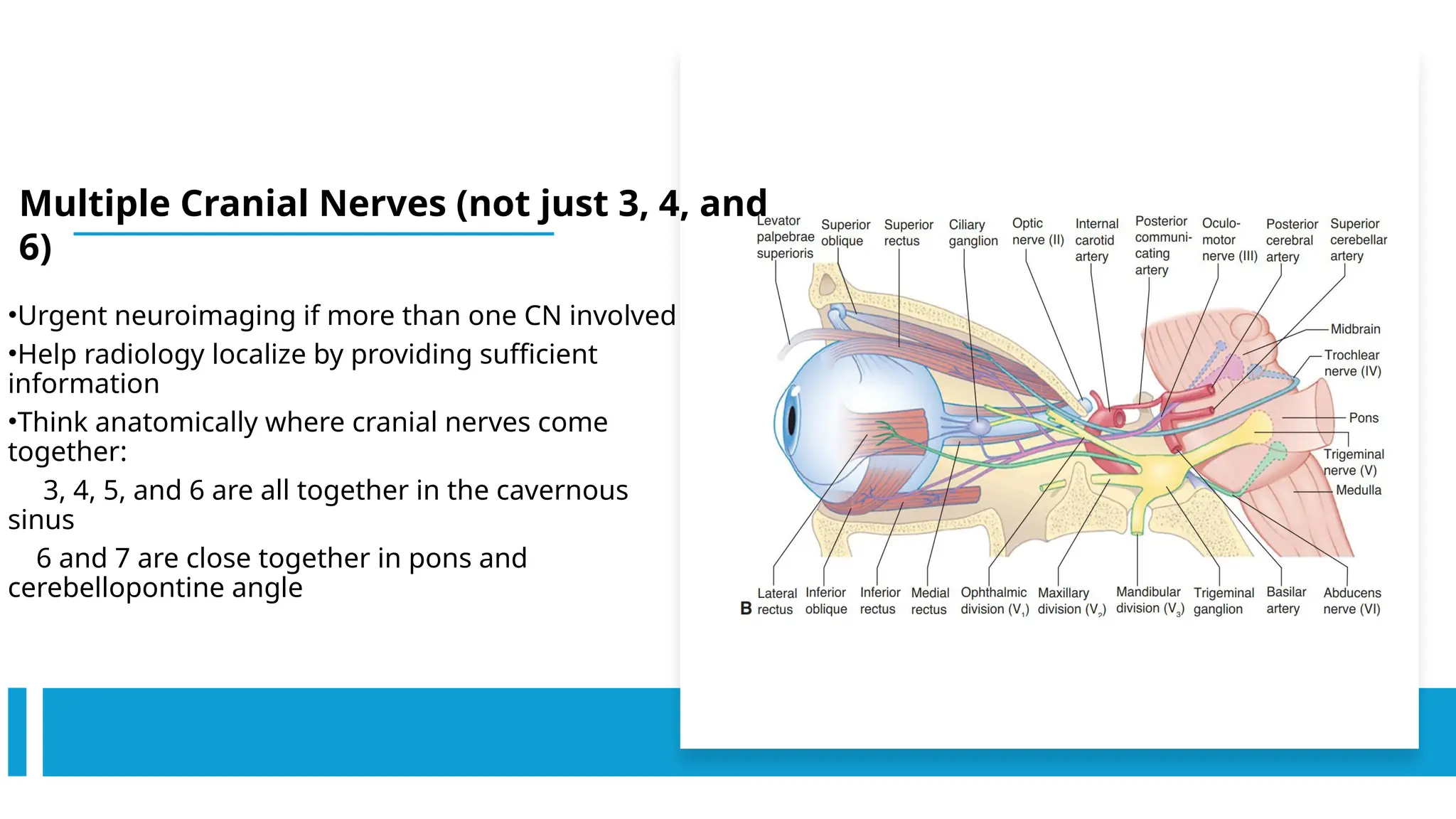
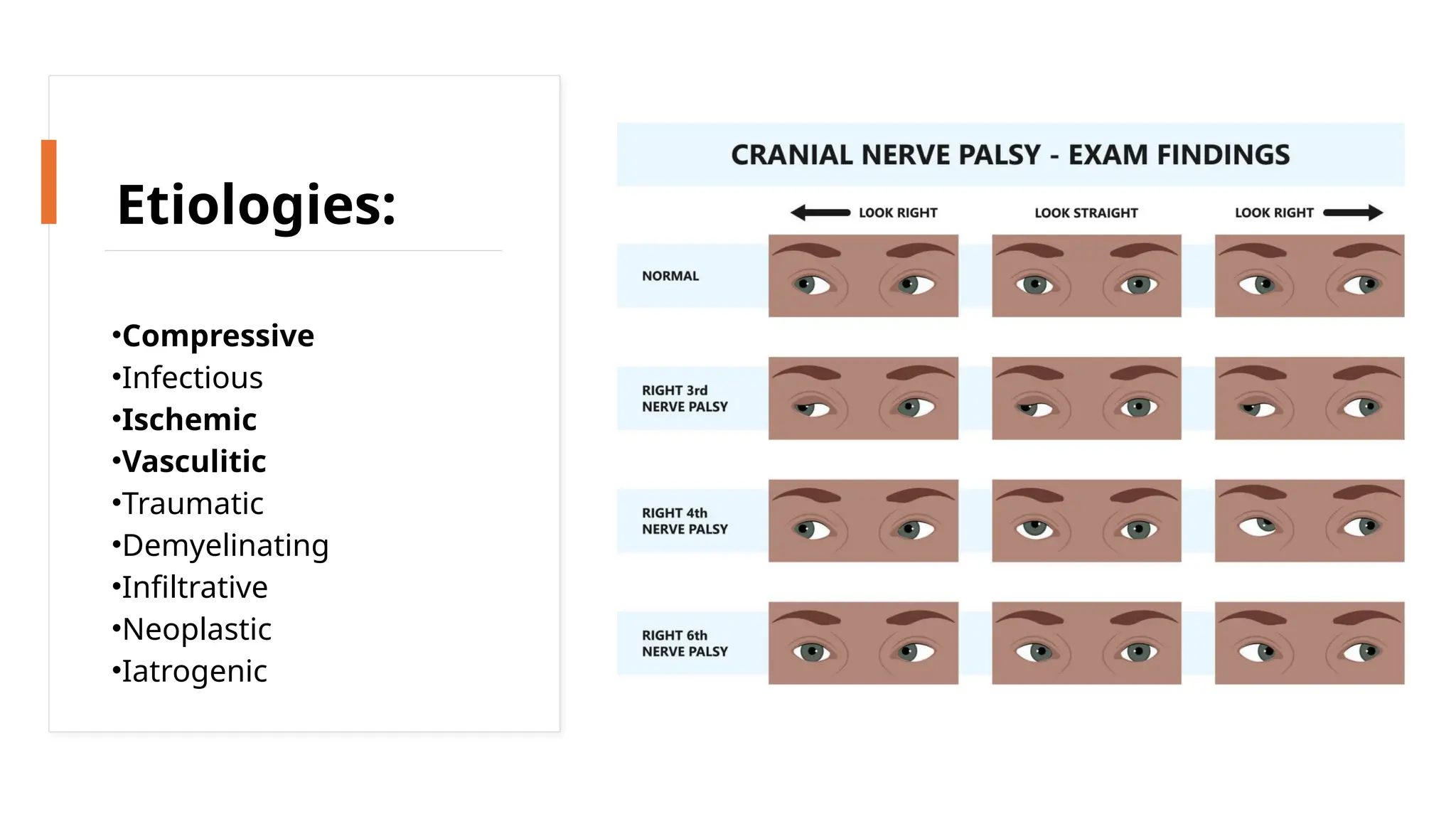
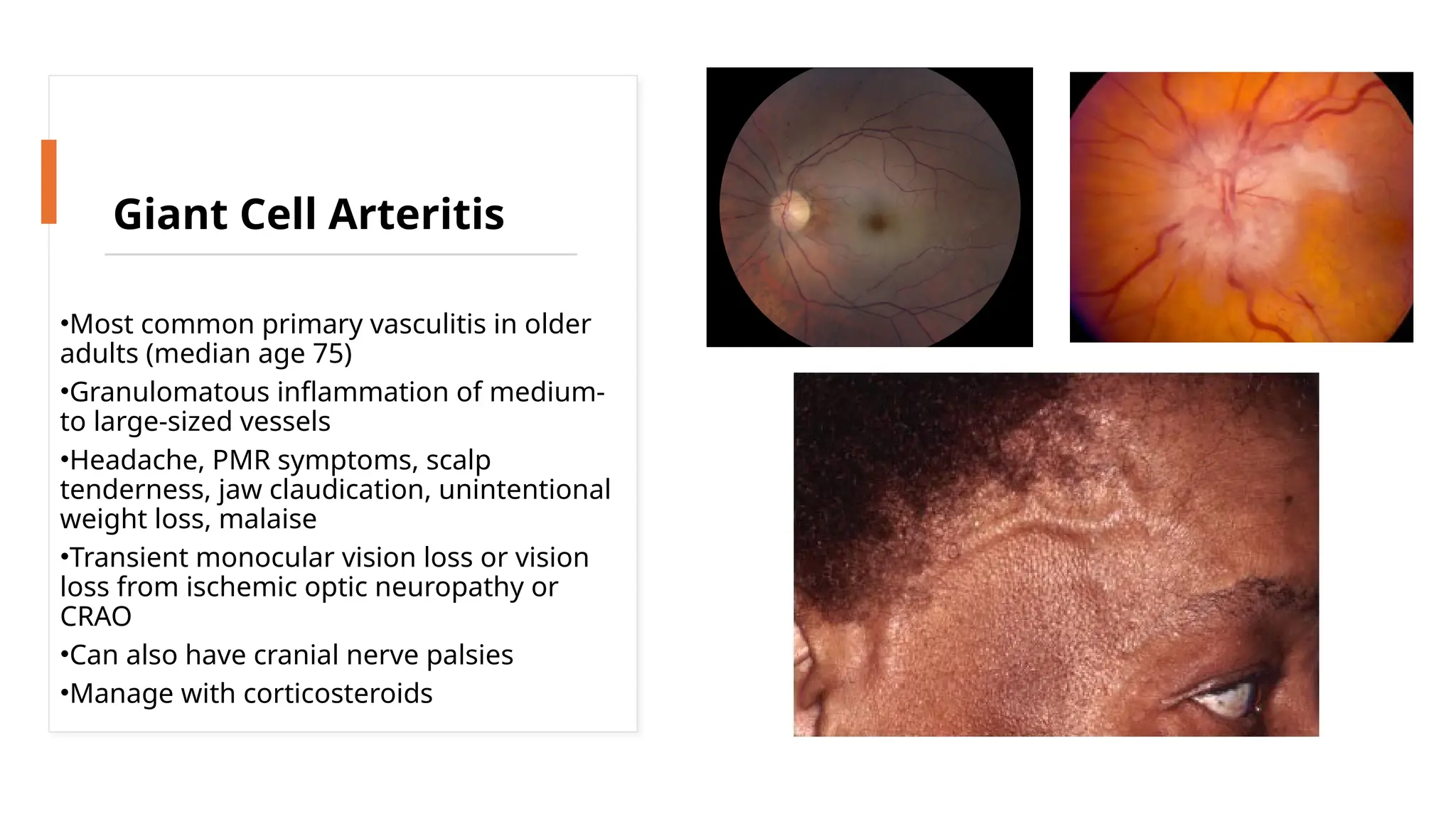
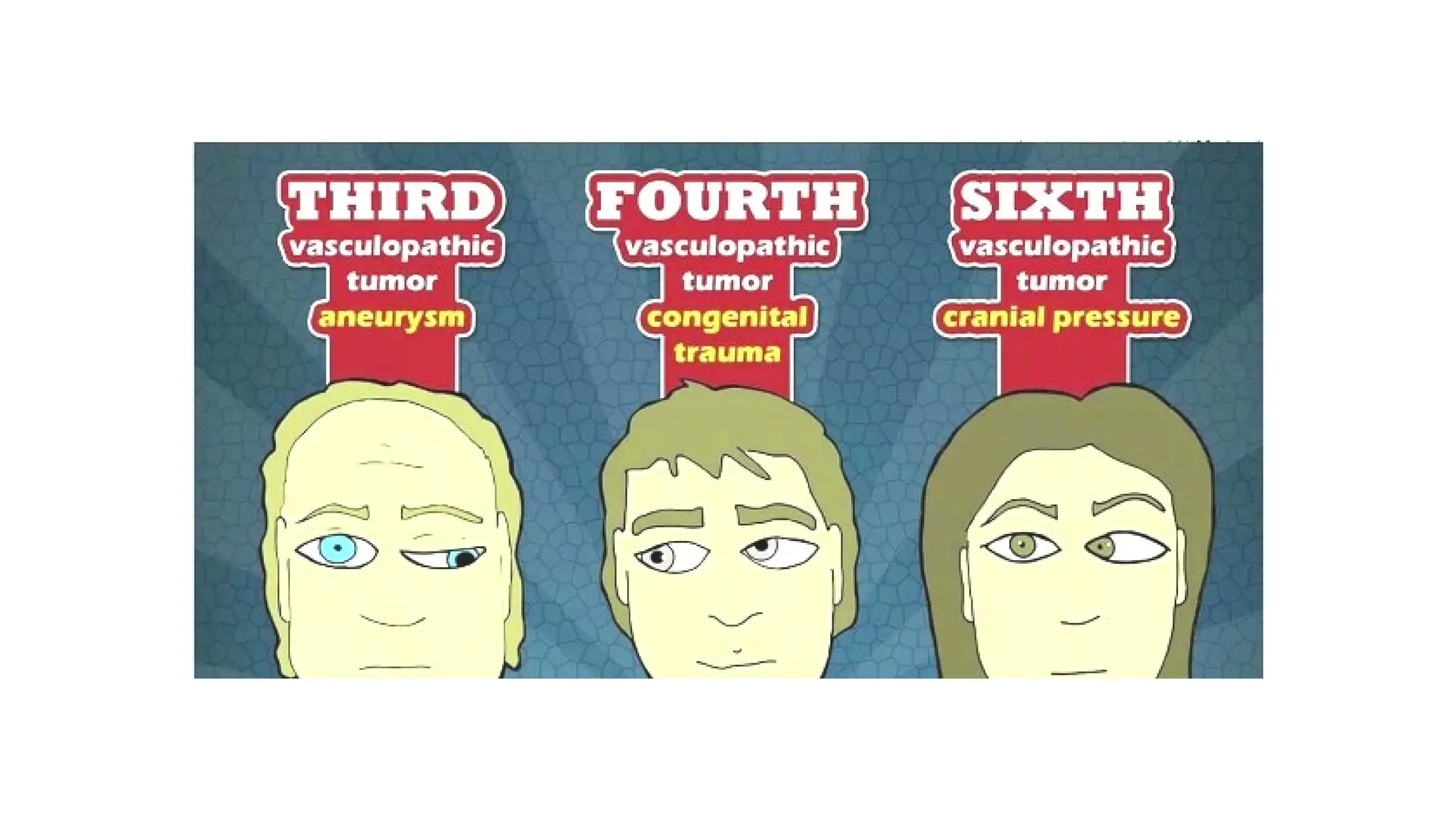
The document provides a detailed overview of the anatomy and clinical implications of cranial nerves III (oculomotor), IV (trochlear), and VI (abducens), highlighting their pathways, vulnerabilities, and associated conditions like cranial nerve palsies. It discusses the etiologies of cranial nerve palsies, diagnosis through imaging techniques, and specific tests to assess nerve function and eye movements. The document emphasizes the importance of understanding these nerves for accurate diagnosis and treatment of related neurological issues.