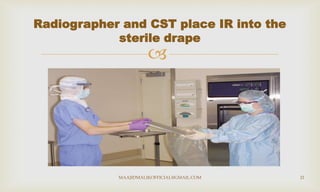
The document discusses the roles and responsibilities of radiographers working in an operating room setting. It describes the surgical team, including sterile and non-sterile team members. Proper surgical attire is emphasized, including protective eyewear, masks, shoe covers, caps, gloves, and identification badges. Strict adherence to hygiene protocols and universal precautions when handling image receptors is crucial to avoid contamination and ensure patient safety.