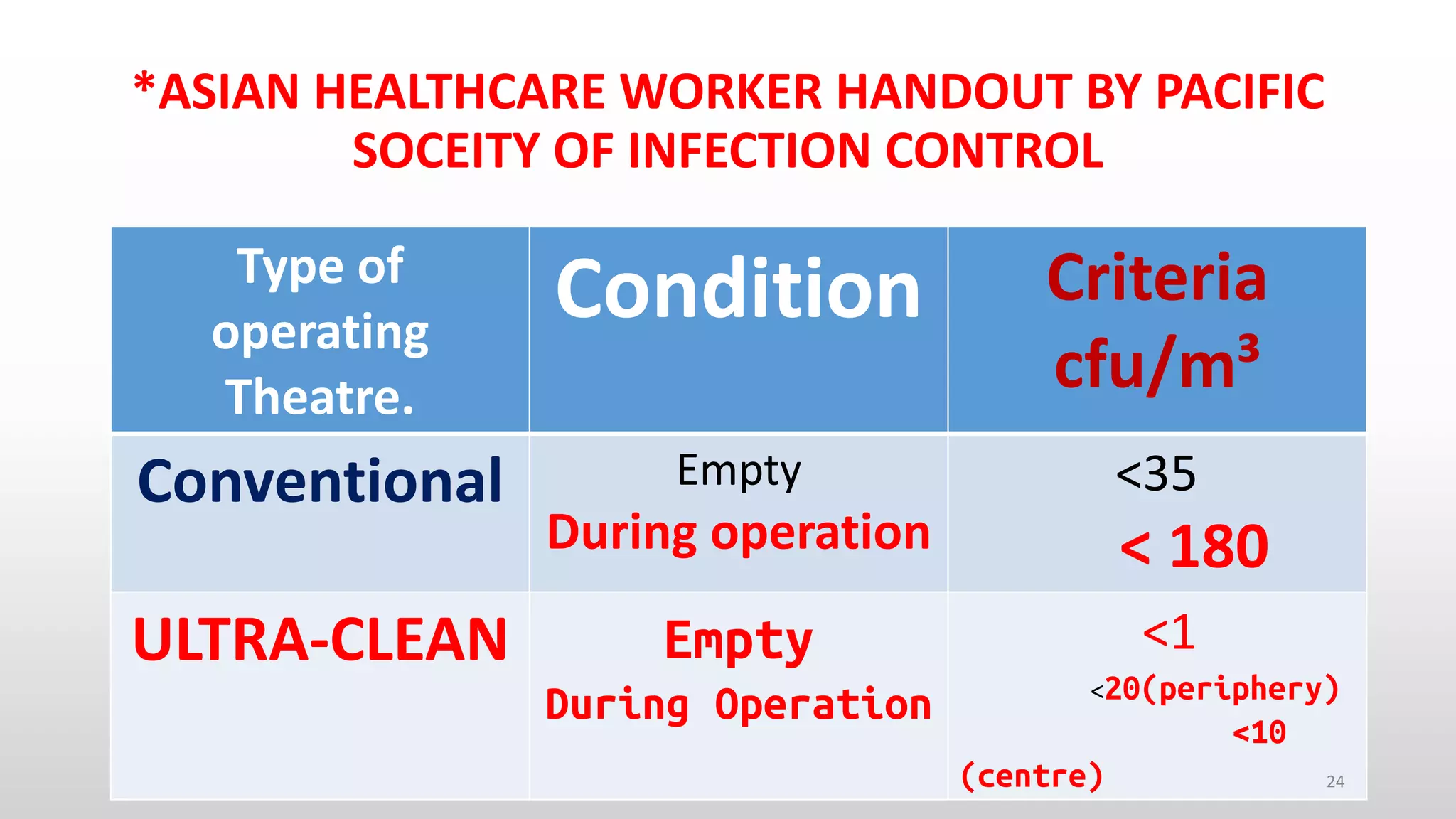
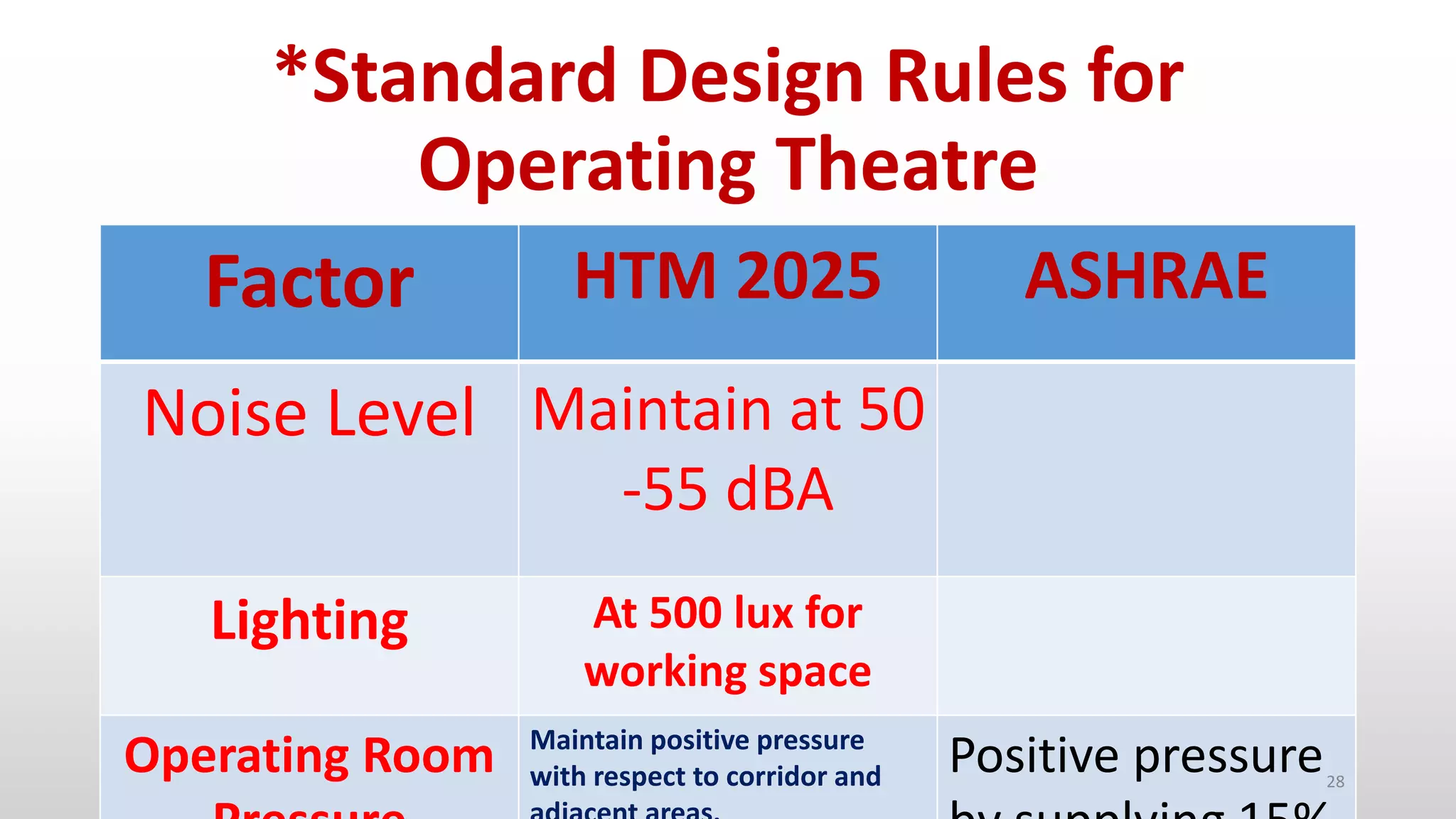
This document discusses the need for standardized operation theater protocols and practices in India to improve safety and reduce infections. It provides an overview of key factors that influence surgical site infections and international standards for operation theater design including air filtration levels, air changes per hour, temperature, humidity and positive pressurization. The document emphasizes establishing standards for documentation, recording surgical procedures, and microbiological surveillance of operation theaters to enhance patient safety.