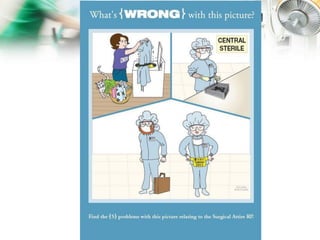
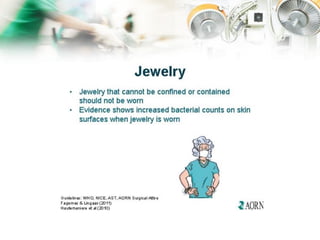
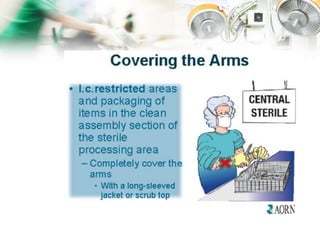
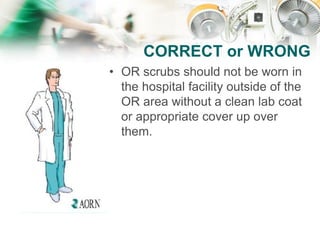
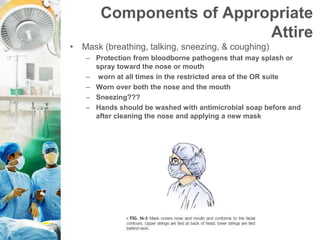
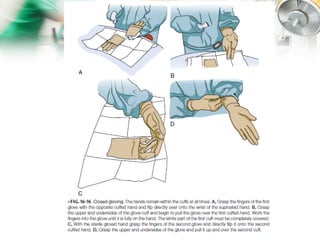
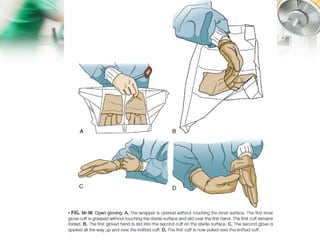
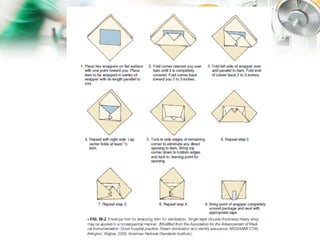
The document describes the roles and responsibilities of the surgical team which includes the surgeon, anesthesiologist, surgical assistants, scrub nurse, and circulating nurse. It explains that the surgical team works together to ensure patient safety and care during surgical procedures. Appropriate attire and aseptic technique are essential to prevent infection and maintain a sterile environment in the operating room.