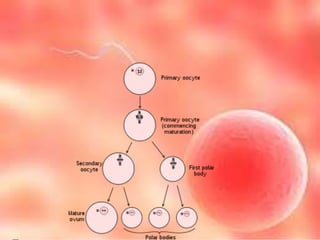
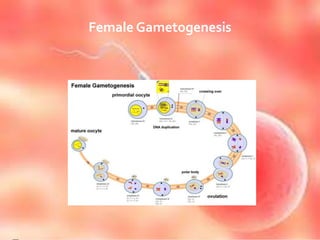
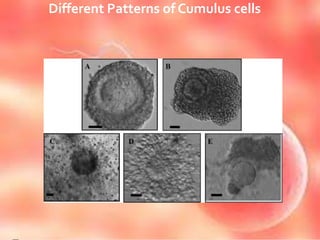
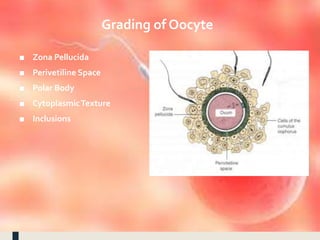
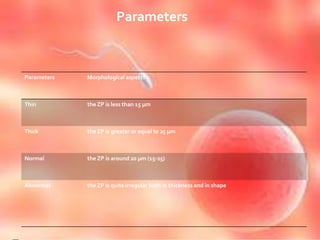
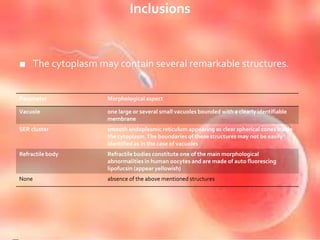
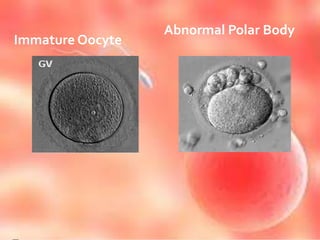
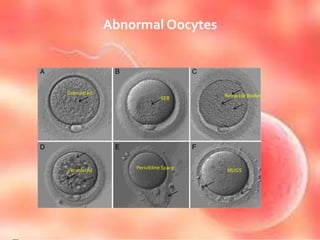
The document provides a detailed overview of oogenesis, the process of female gametogenesis in mammals, outlining the development of oocytes from primordial germ cells through various stages until maturation into ovum. Key processes mentioned include oocytogenesis, ootidogenesis, and folliculogenesis, which describe the transformation and maturation of oocytes and ovarian follicles. Additionally, the document discusses the structural characteristics of oocytes, abnormalities that can occur, and the role of maternal contributions in embryonic development.