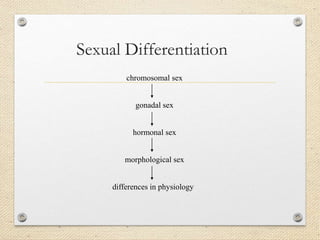
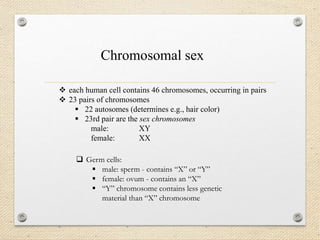
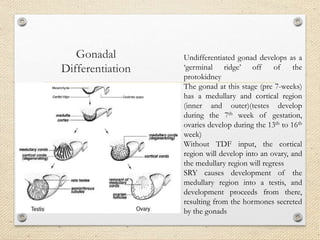
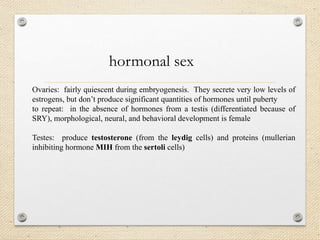
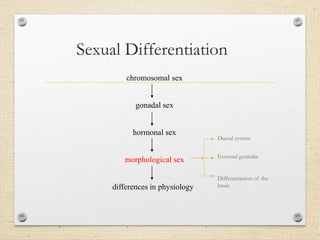
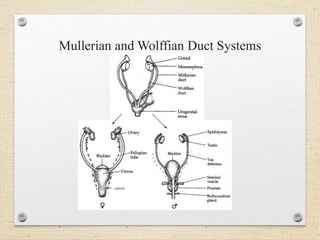
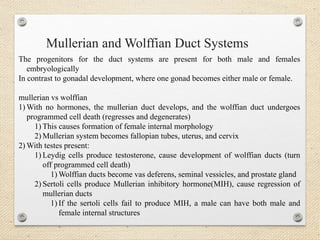
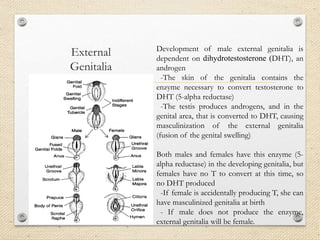
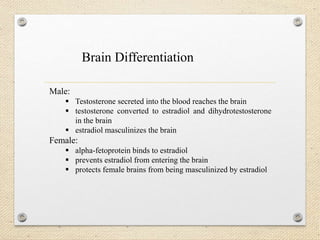
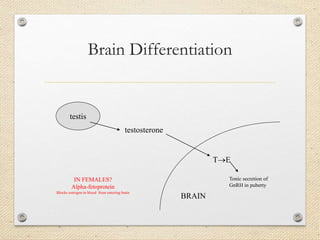
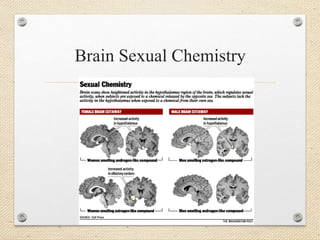
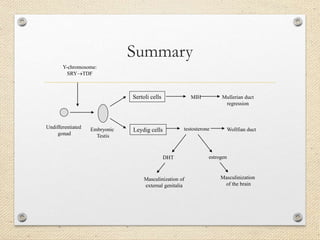
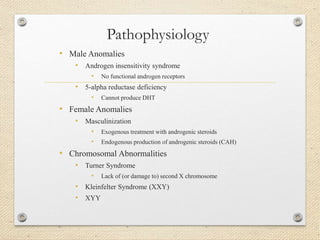
Sexual differentiation in humans occurs through a multi-step process determined by chromosomal, gonadal, hormonal, and morphological sex. The presence or absence of the SRY gene on the Y chromosome triggers testis or ovary development from the initially undifferentiated gonad. The testes secrete testosterone and Müllerian inhibiting hormone which masculinize the internal and external genitalia as well as the brain, preventing female development. In the absence of these hormones, the individual develops along female lines. Disorders can occur at each stage of differentiation, resulting in intersex conditions or abnormalities in sexual development.