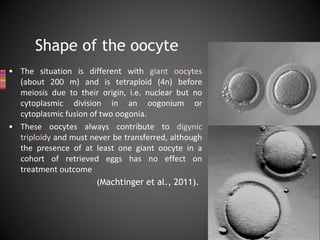
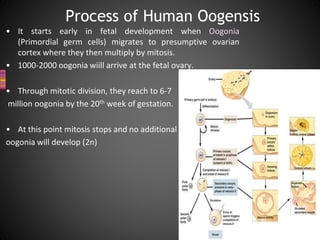
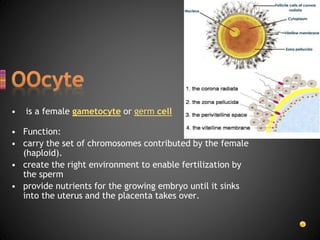
This document summarizes key aspects of human oogenesis and oocyte quality assessment. It describes the process of oogenesis, including formation of follicles in the ovaries and maturation of oocytes. It also discusses morphological features used to assess oocyte quality, such as the cumulus-oocyte complex, nuclear maturity, size and shape, the zona pellucida, polar body morphology, and perivitelline space. While some studies found correlations between certain morphological features and development outcomes, others found no significant correlations. Overall assessment of oocyte quality relies on evaluating multiple morphological characteristics.








![• Morphological oocyte assessment is based on the aspects of :
1- Cumulus-corona cells
2- if denudation is performed
3- Oocyte morphology : a rapid evaluation using an inverted microscopic is
also performed after denudation;
the cytoplasm,
the perivitelline space,
the first polar body,
the zona pellucida.
provides very superficial and approximate information about;
the stage of development [germinal vesicle, metaphase I (MI) or MII phase]
the quality [degenerative signs in the cytoplasm, polar body (PB) or zona
pellucida]
Oocyte quality assessment](https://image.slidesharecdn.com/guidelines-160429181927/85/Oocyte-Morphology-assessment-14-320.jpg)