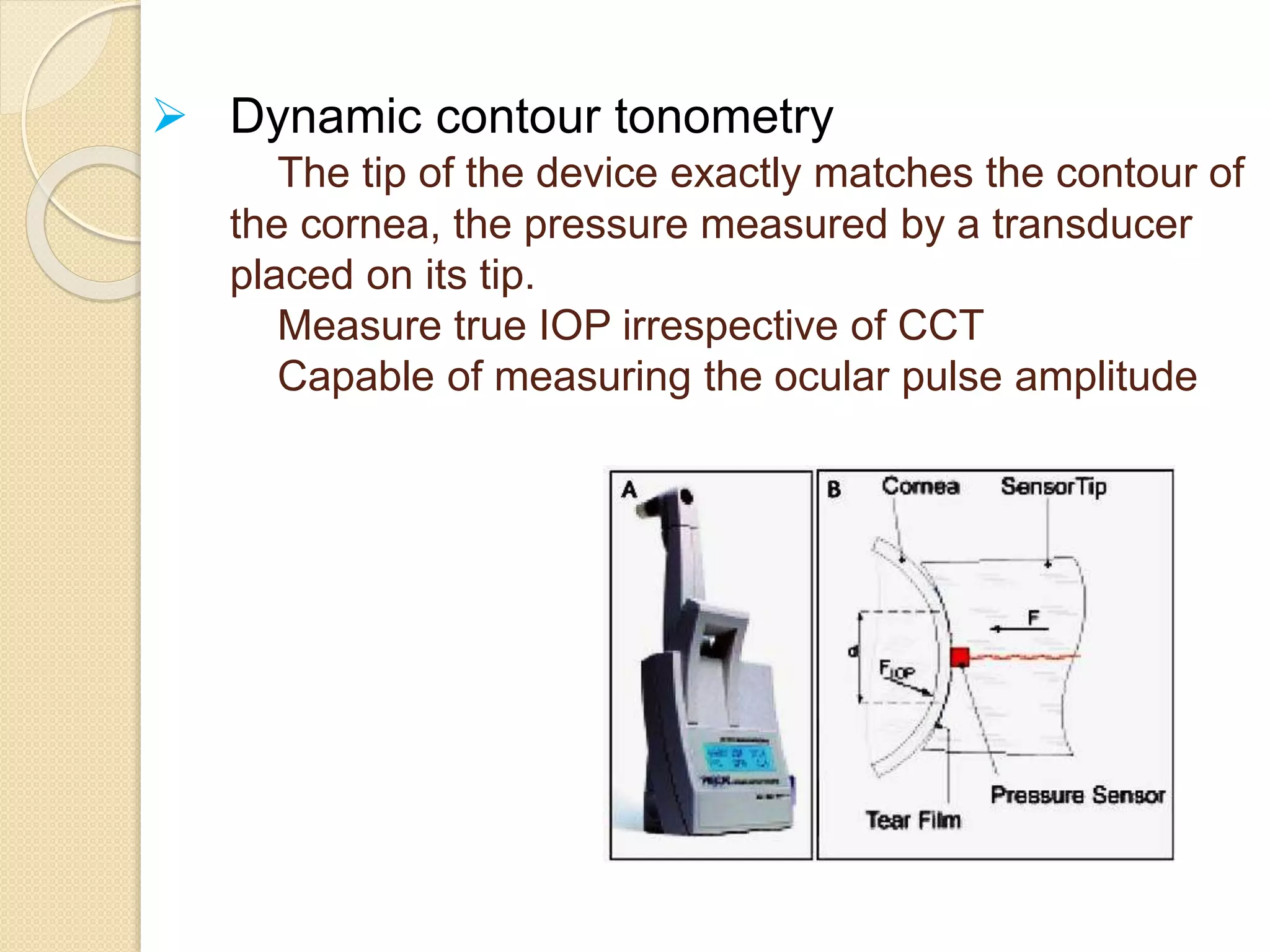
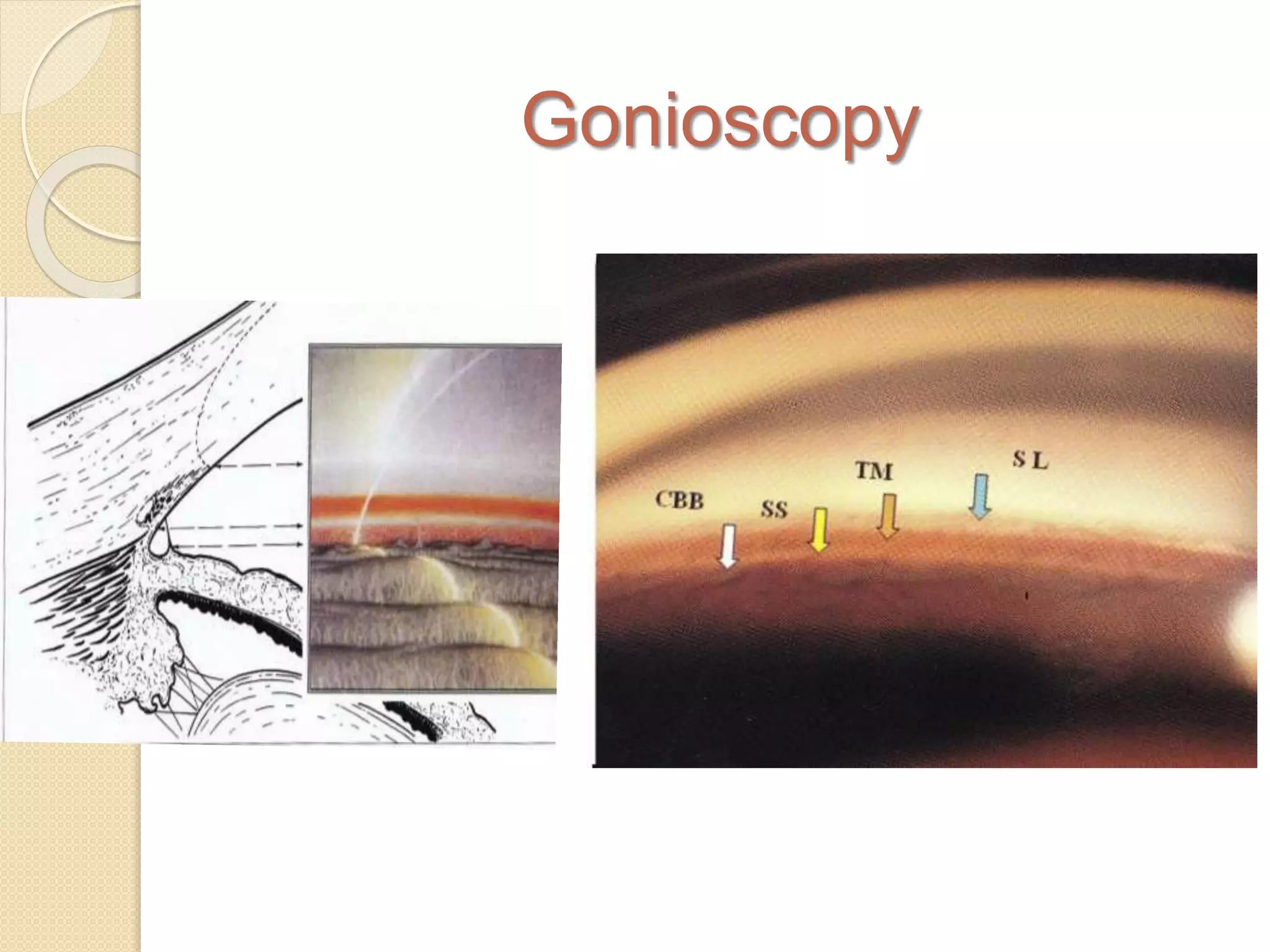
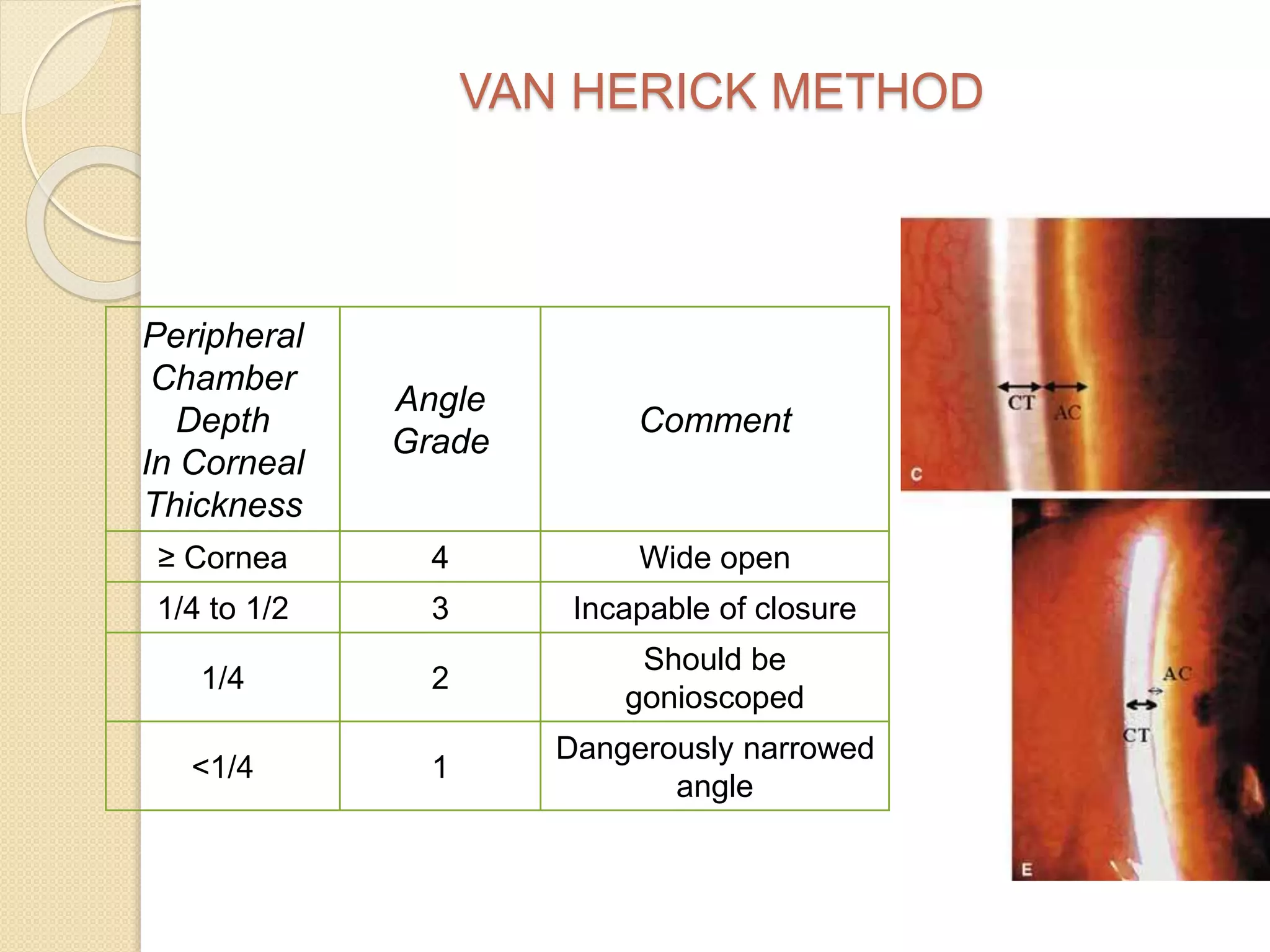
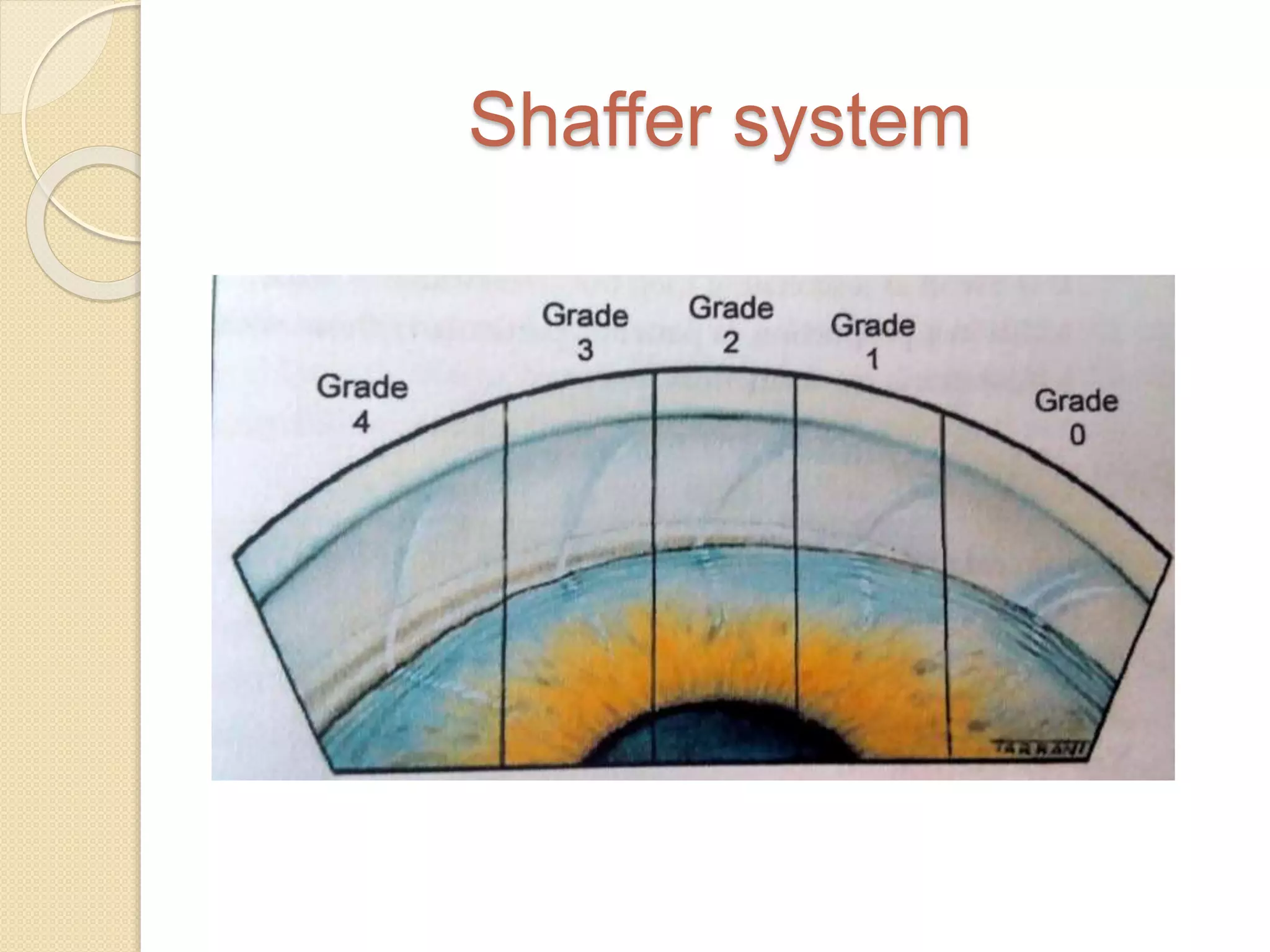
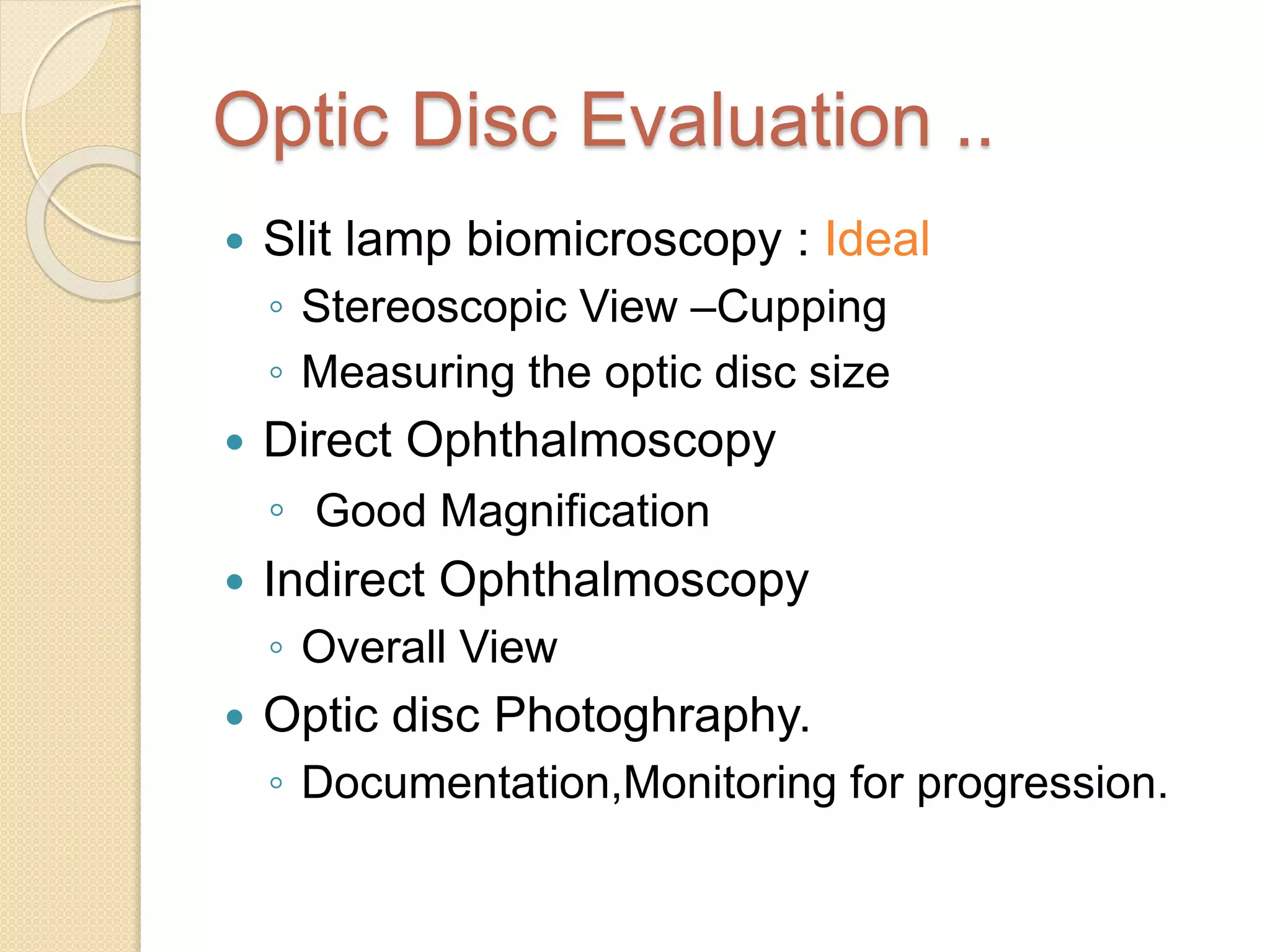
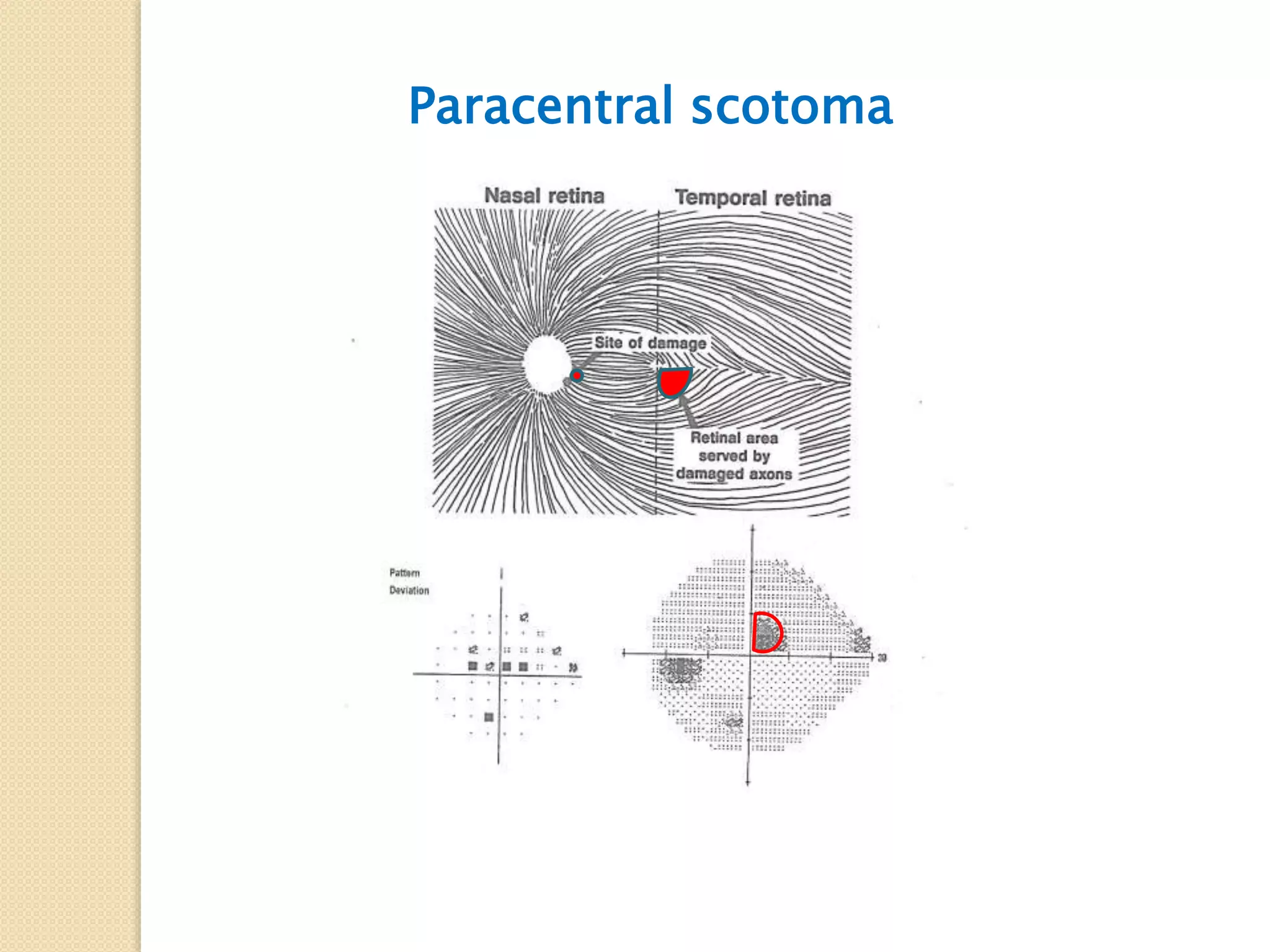
This document provides an overview of evaluating a glaucoma patient. It discusses the classification, clinical evaluation, history, clinical examination including slit lamp biomicroscopy, tonometry, gonioscopy, optic disc evaluation, visual field testing, and OCT. Classification is based on whether glaucoma is congenital or acquired, primary or secondary, open angle or angle-closure. The clinical evaluation aims to diagnose the specific form of glaucoma, determine severity, and assess disease progression. A thorough history and clinical examination are essential for appropriate glaucoma management.