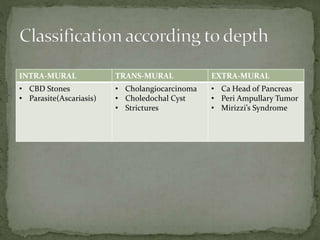
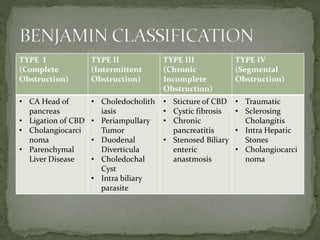
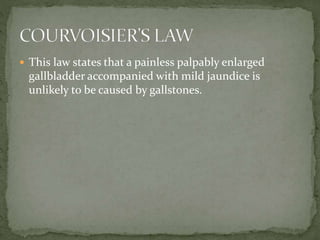
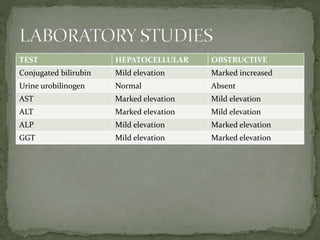
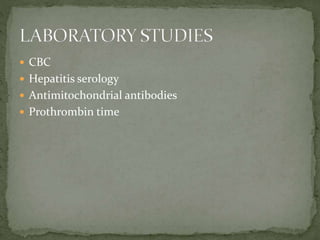
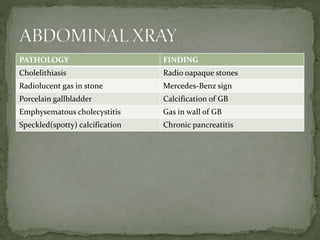
The document discusses jaundice, its types, causes, symptoms, and diagnostic methods, highlighting the importance of identifying the underlying issues. It provides detailed insights into the management and treatment of biliary conditions, including various diagnostic procedures and interventions. Additionally, it outlines the relationship between jaundice and conditions like gallbladder disease, emphasizing the need for timely treatment to prevent complications.























![ Center SA. Diseases of the gallbladder and biliary tree. Vet Clin North
Am Small Anim Pract. 2009 May. 39(3):543-98. [QxMD MEDLINE
Link].
Marrelli D, Caruso S, Pedrazzani C, et al. CA19-9 serum levels in
obstructive jaundice: clinical value in benign and malignant
conditions. Am J Surg. 2009 Sep. 198(3):333-9. [QxMD MEDLINE Link].
Bektas M, Dokmeci A, Cinar K, et al. Endoscopic management of
biliary parasitic diseases. Dig Dis Sci. 2010 May. 55(5):1472-8. [QxMD
MEDLINE Link].
Zhu AX, Hong TS, Hezel AF, Kooby DA. Current management of
gallbladder carcinoma. Oncologist. 2010. 15(2):168-81. [QxMD
MEDLINE Link]. [Full Text].
O'Connell W, Shah J, Mitchell J, et al. Obstruction of the biliary and
urinary system. Tech Vasc Interv Radiol. 2017 Dec. 20(4):288-
93. [QxMD MEDLINE Link].](https://image.slidesharecdn.com/obstructivejaundice-230531132406-537681c3/85/OBSTRUCTIVE-JAUNDICE-pptx-38-320.jpg)
