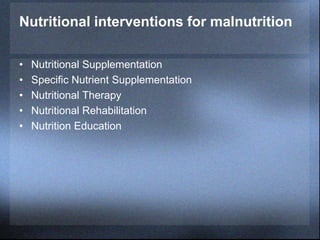
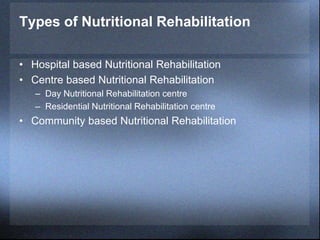
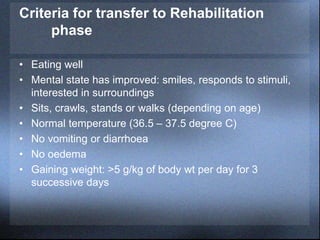
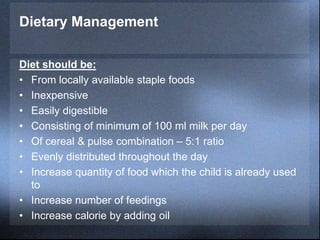
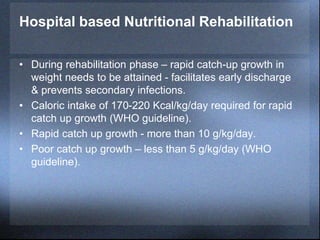
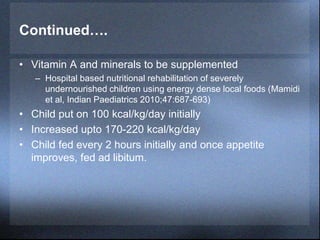
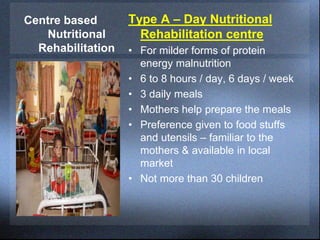
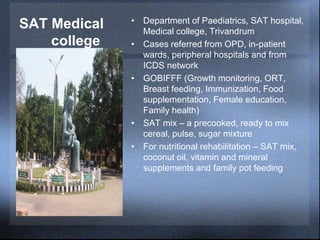
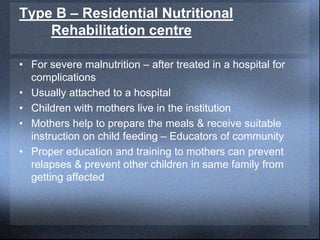
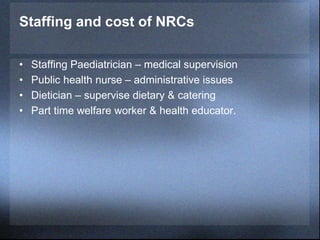
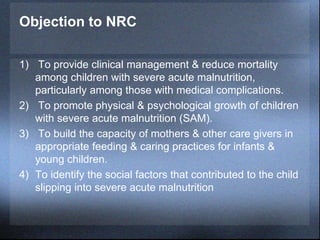
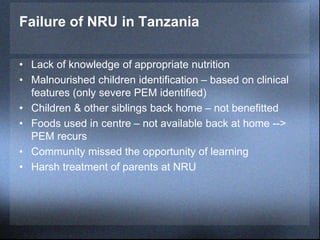
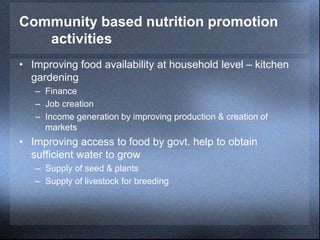
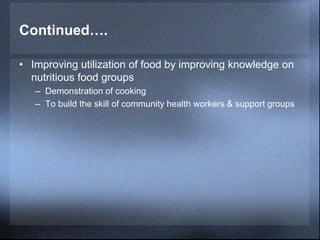
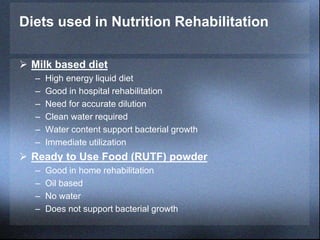
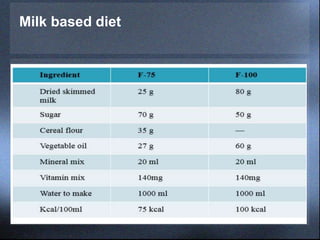
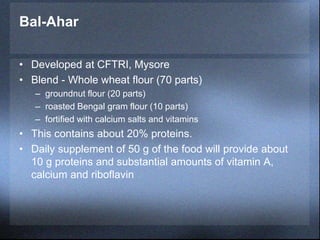
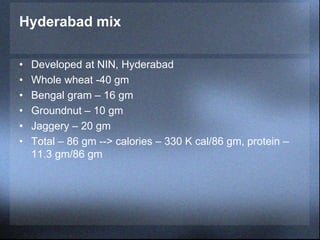
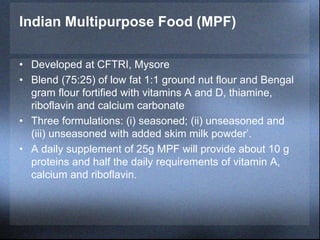
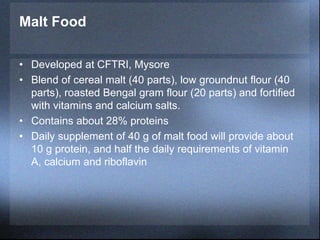
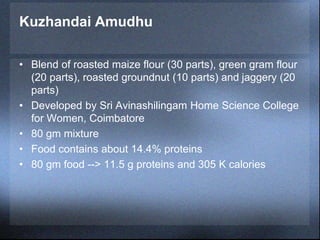
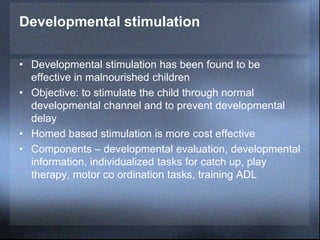
This document discusses various approaches to nutritional rehabilitation for malnutrition, including hospital-based, centre-based, and community-based rehabilitation. It describes diets used in rehabilitation such as milk-based diets and ready-to-use therapeutic foods. It also discusses criteria for transferring patients to rehabilitation, staffing of rehabilitation centres, community nutrition programs, and developmental stimulation techniques.