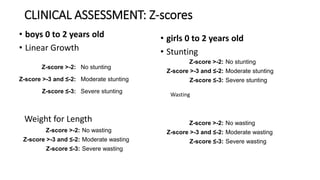
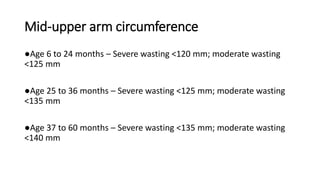
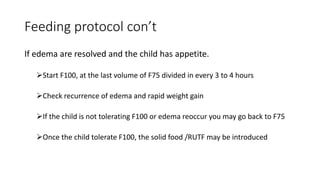
The document discusses malnutrition, which includes undernutrition and overnutrition, detailing its types, global prevalence, and clinical assessment methods. It emphasizes the significance of malnutrition in children, highlighting specific nutrient deficiencies and criteria for diagnosing acute malnutrition. Management strategies for severe and complicated malnutrition in children are outlined, including feeding protocols, prevention of complications, and the importance of parental involvement in care.





























![References
• Phillips SM, Jensen C, Editor S, Motil KJ, Editor D, Hoppin AG. Micronutrient
deficiencies associated with malnutrition in children Micronutrient deficiencies
associated with malnutrition in children. 2013;1(table 1):1–15.
• Praveen S Goday M. Malnutrition in children in resource-limited countries:
Clinical assessment - UpToDate. UpToDate [Internet]. 2019;5. Available from:
https://www.uptodate.com/contents/malnutrition-in-children-in-resource-limited-
countries-clinical-assessment%0Ahttps://www.uptodate.com/contents/malnutrition-
in-children-in-resource-limited-countries-clinical-assessment/print
• WHO. Girls z-scores. 2006;15. Available from:
http://www.who.int/childgrowth/standards/LFA_girls_0_13_percentiles.pdf%5Cnpape
rs2://publication/uuid/8A8286DD-5E8A-4952-AAFF-8A0275597782
• WHO. WHO | Chart catalogue. Who. 2010.
• Ashworth A, Schofield C. Book Review: Guidelines for the Inpatient Treatment of
Severely Malnourished Children. Food Nutr Bull. 2005;26(2):245–245.
• Goday P. Malnutrition in children in resource-limited countries: Clinical
assessment - UpToDate [Internet]. UpToDate. 2019. Available from:
https://ezproxy.ufm.edu:2053/contents/malnutrition-in-children-in-resource-limited-
countries-clinical-assessment?search=malnutrition in
children&source=search_result&selectedTitle=1~150&usage_type=default&display_ra
nk=1](https://image.slidesharecdn.com/malnutritioninpediatrics-191216171204/85/Malnutrition-in-pediatrics-33-320.jpg)
![References
• USAID. Rwanda : Nutrition Profile. American [Internet]. 2014;(June):7–10.
Available from:
https://www.usaid.gov/sites/default/files/documents/1864/Rwanda-Nutrition-
Profile-Mar2018-508.pdf
• Trehan I, Manary M. Management of complicated severe acute
malnutrition in children in resource-limited countries. UpToDate.com
[Internet]. 2017;1–22. Available from: https://0-
www.uptodate.com.innopac.wits.ac.za/contents/management-of-complicated-
severe-acute-malnutrition-in-children-in-resource-limited-
countries?source=search_result&search=severe
malnutrition&selectedTitle=1~150
• Trehan I, Manary M. Management of complicated severe acute
malnutrition in children in resource-limited countries [Internet].
UpToDate.com. 2017. p. 1–22. Available from: https://0-
www.uptodate.com.innopac.wits.ac.za/contents/management-of-complicated-
severe-acute-malnutrition-in-children-in-resource-limited-
countries?source=search_result&search=severe
malnutrition&selectedTitle=1~150
• Airlines S. 済無No Title No Title. J Chem Inf Model. 2013;53(9):1689–99.](https://image.slidesharecdn.com/malnutritioninpediatrics-191216171204/85/Malnutrition-in-pediatrics-34-320.jpg)