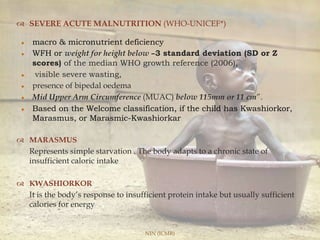
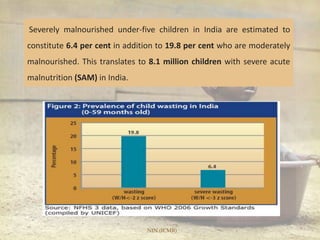
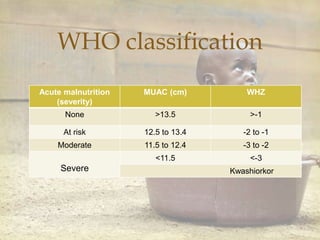
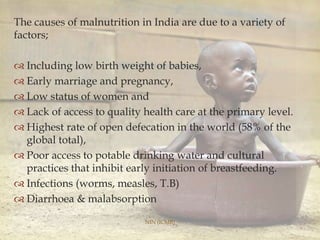
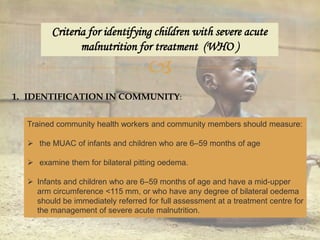
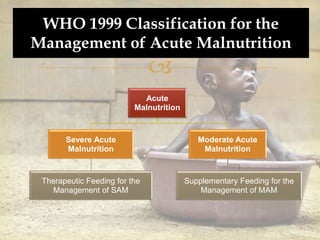
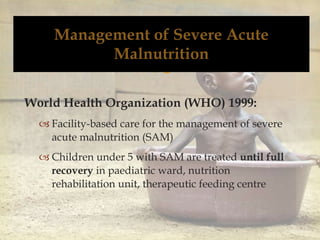
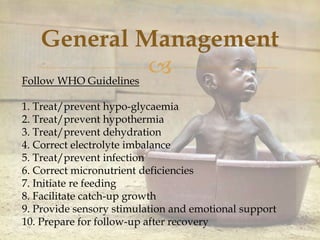
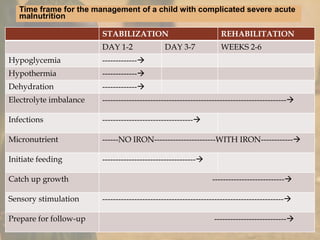
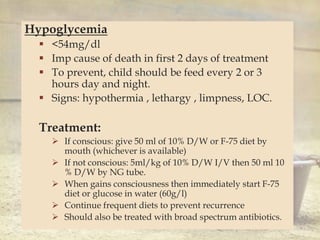
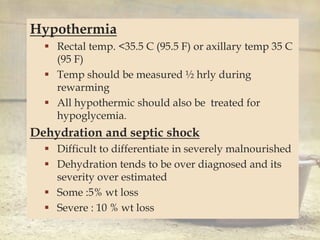
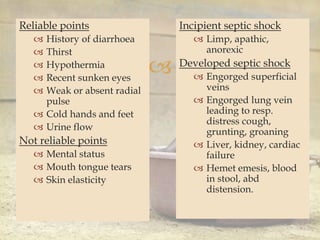
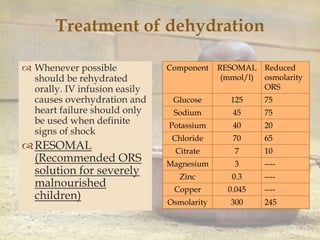
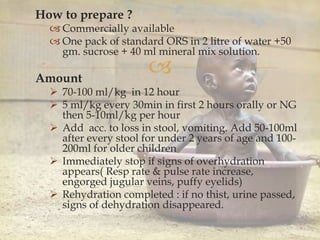
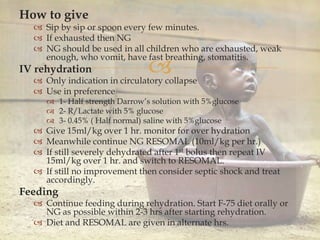
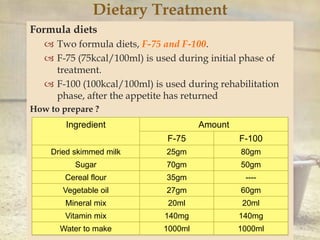
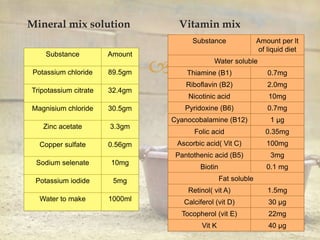
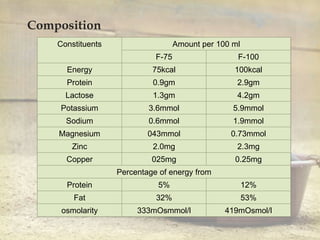
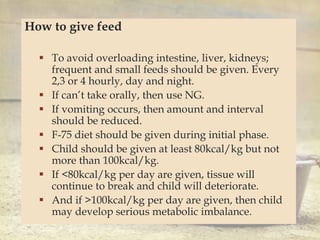
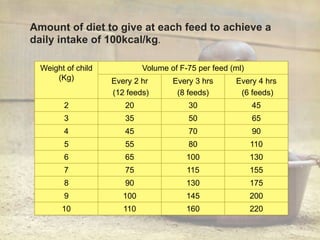
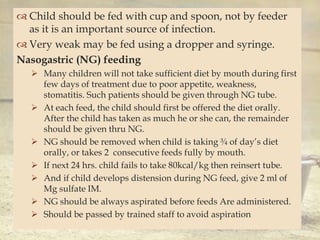
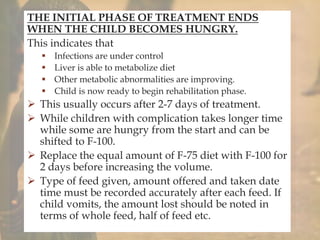
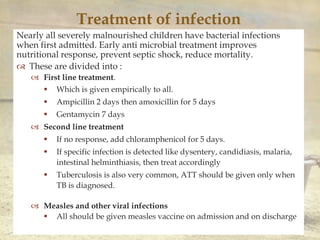
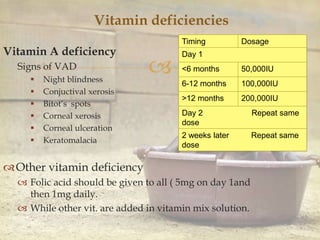
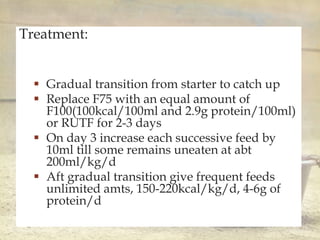
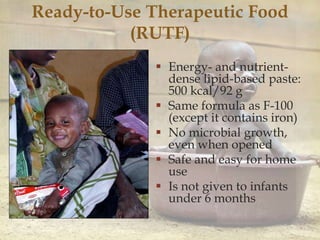
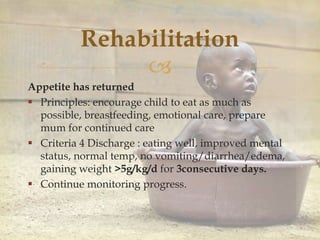
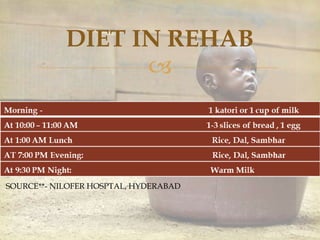
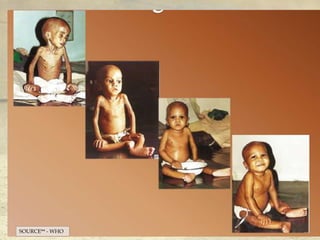
This document provides information on malnutrition definitions, prevalence, causes, admission and discharge criteria, and general management for malnutrition in India from the National Institute of Nutrition (ICMR). It defines severe acute malnutrition and provides WHO criteria for identifying, admitting, and discharging patients. It also outlines the general 10 step management approach including stabilizing hypoglycemia, hypothermia, and infections before beginning rehabilitation with formula diets like F-75 and F-100 to support catch-up growth.