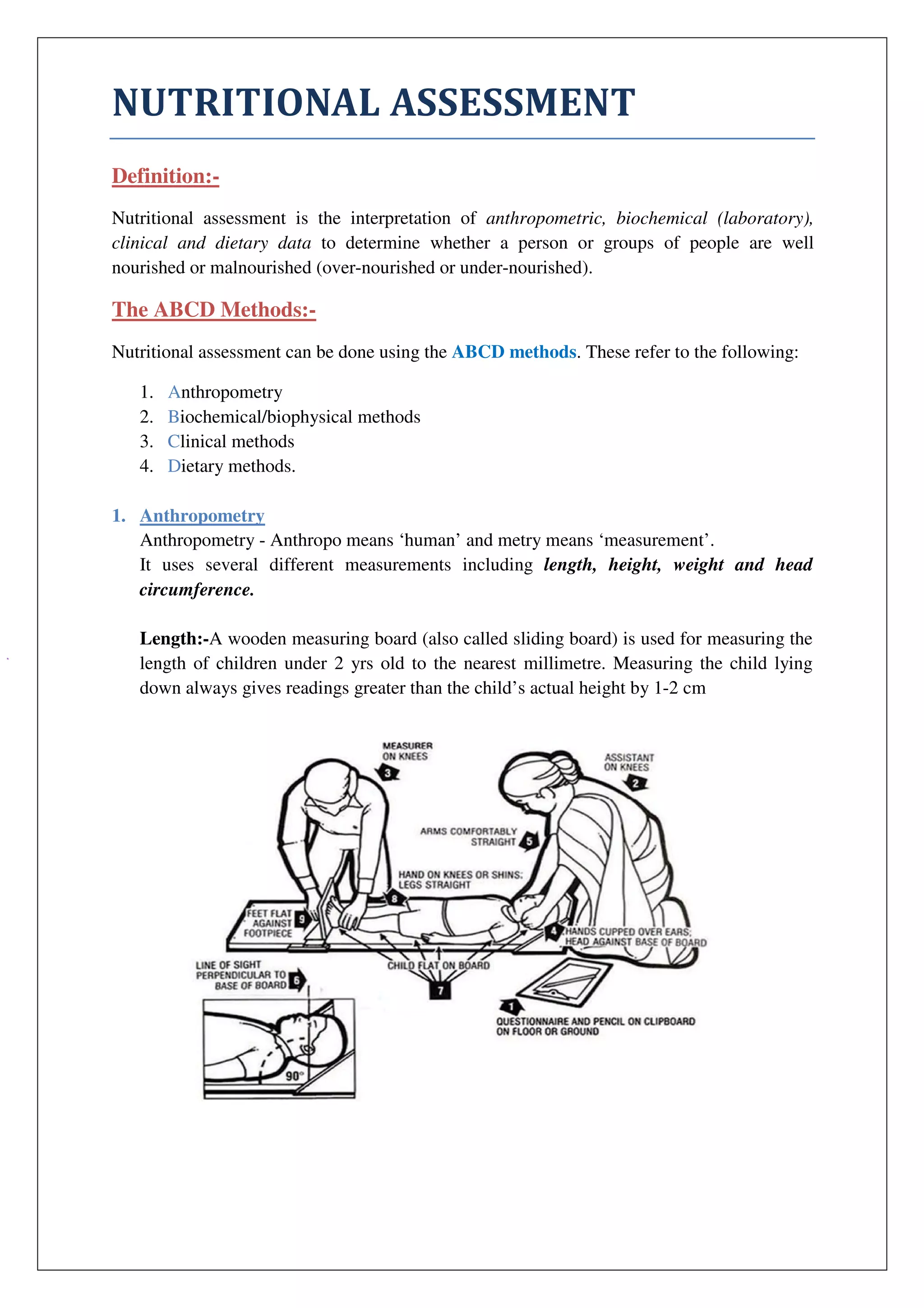
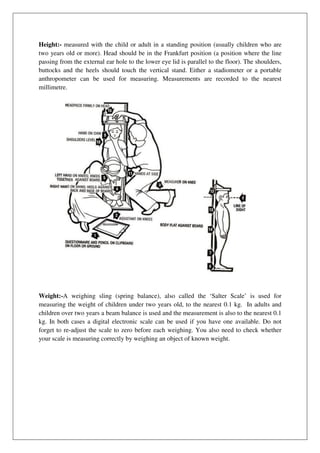
Nutritional assessment involves analyzing anthropometric, biochemical, clinical, and dietary data to determine nutritional status. It can be done using the ABCD methods of anthropometry, biochemical tests, clinical exams, and dietary analyses. Anthropometry includes measuring height, weight, and mid-upper arm circumference to calculate indices like BMI. Biochemical tests measure vitamin and mineral levels. Clinical exams identify signs of deficiency. Dietary analyses evaluate past intake and dietary diversity using 24-hour recalls. Together these methods provide a holistic view of nutritional status.