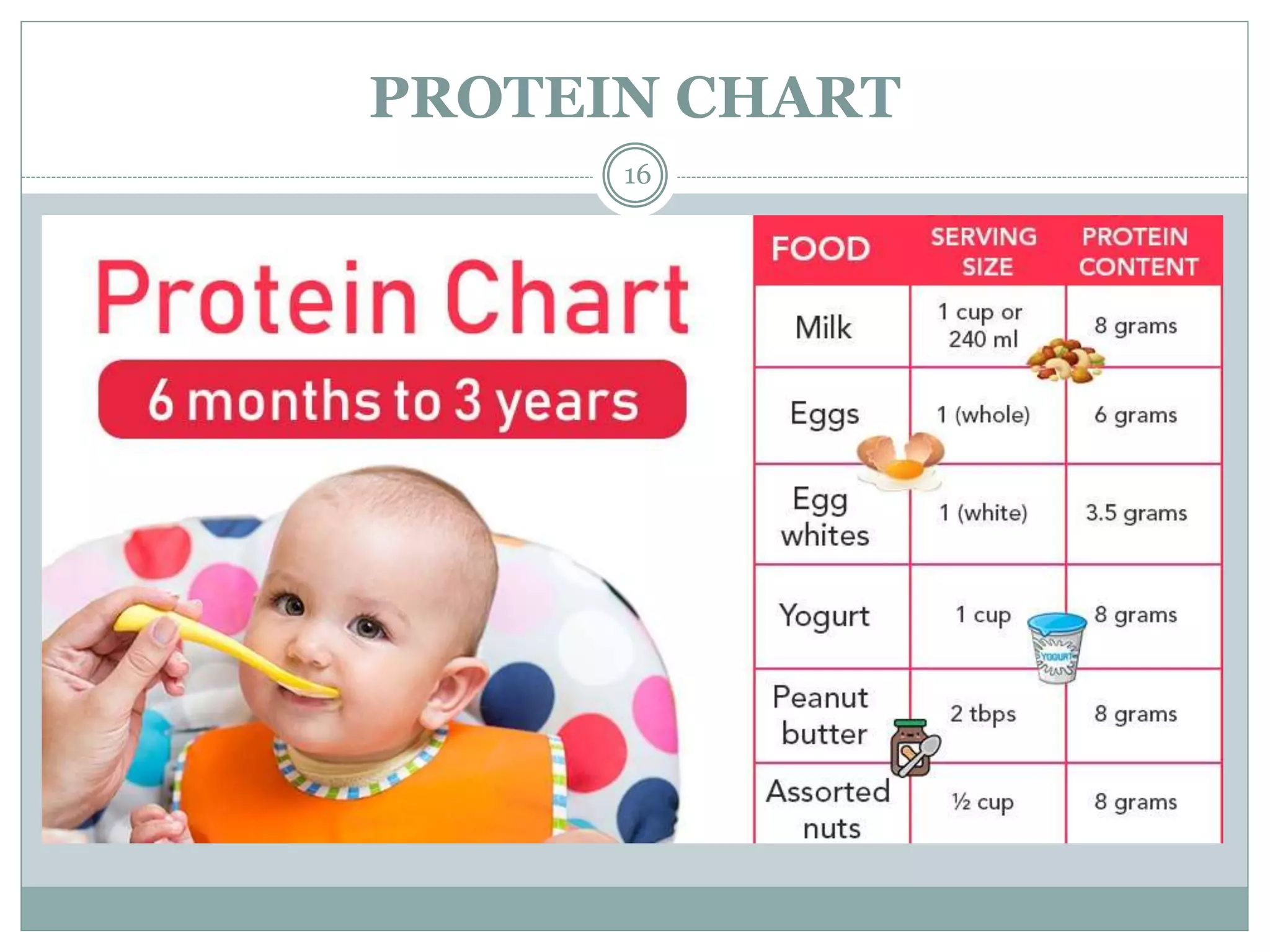
This document provides information on nutrition in infancy. It discusses the adjustment period for newborn infants, growth and development in the first year of life, nutritional requirements, and guidelines for breastfeeding and complementary feeding. The rationale for nutritional requirements is explained for energy, protein, vitamins, minerals, and water. Methods of feeding, sterilization, introducing complementary foods and common disorders in infancy are also outlined. Standard formulas for calculating daily energy requirements in infants of different ages are presented. The document concludes with an overview of relevant policies and programs to support infant nutrition and health in India.