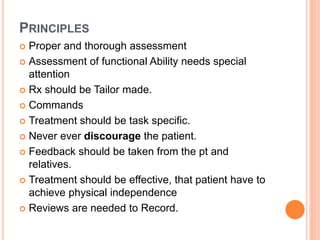
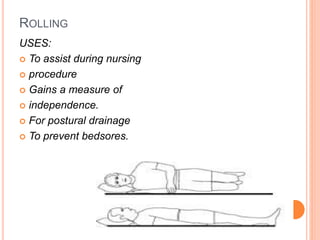
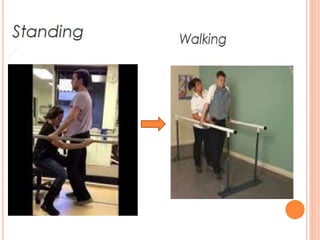
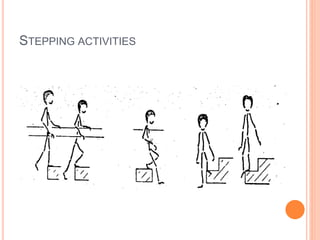
Functional re-education aims to retrain patients' movements and activities that they already know but cannot properly perform due to illness or injury. The goal is to increase independence through a tailored program of progressive exercises. Exercises may include rolling, sitting, kneeling, standing, and walking activities. Principles include thorough assessment, task-specific treatment, and avoiding discouragement to build confidence and independence over time.