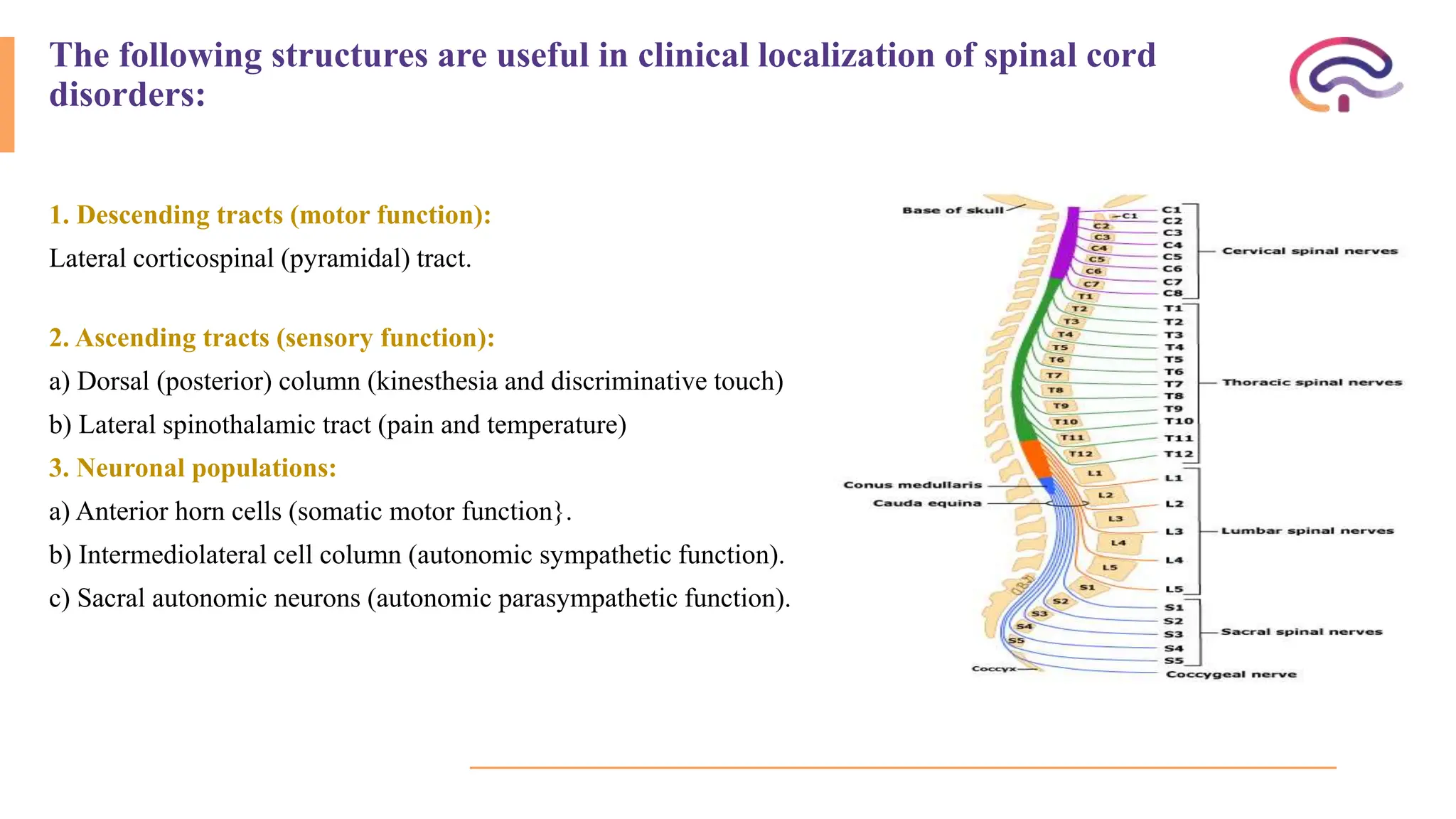
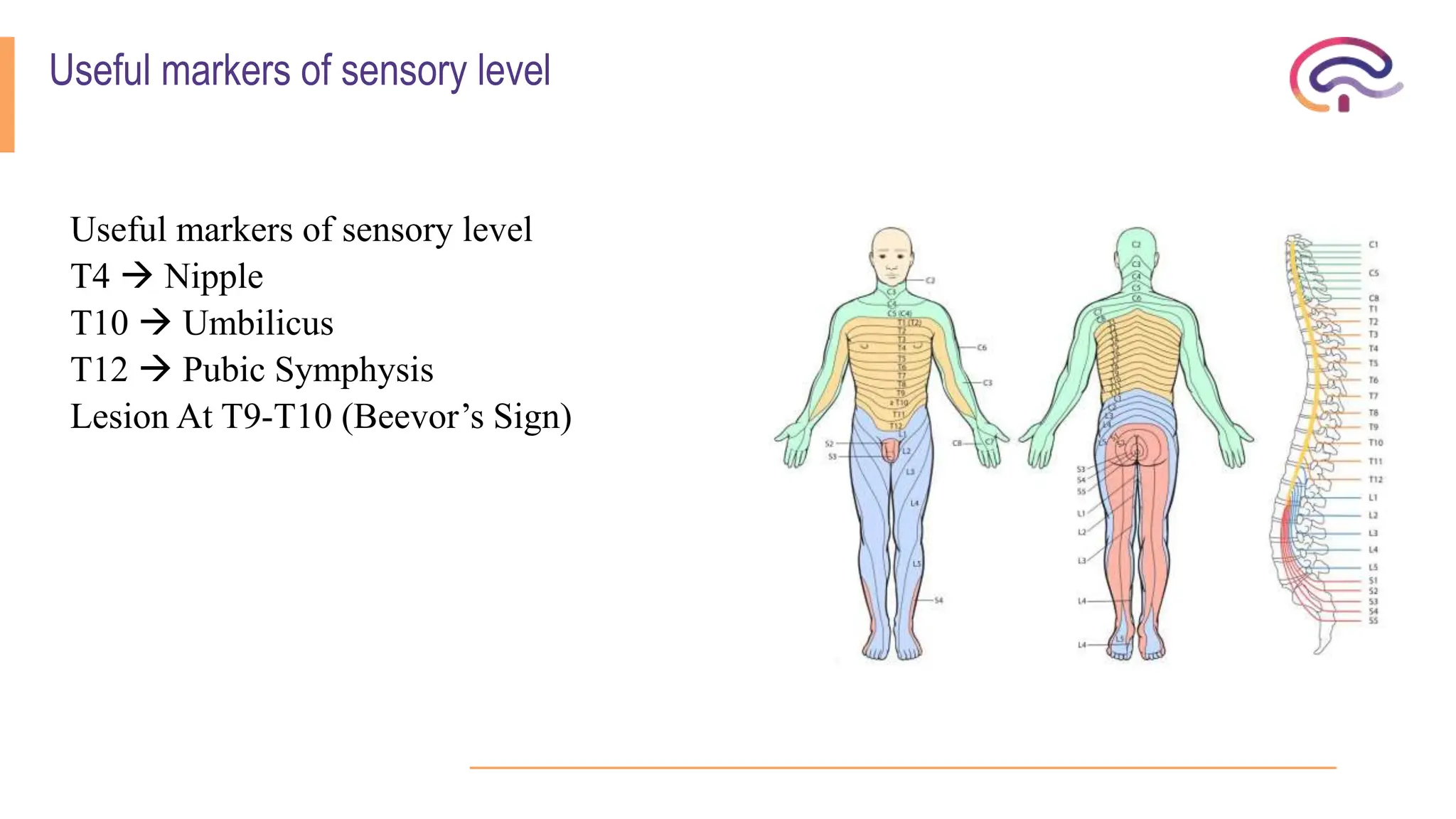
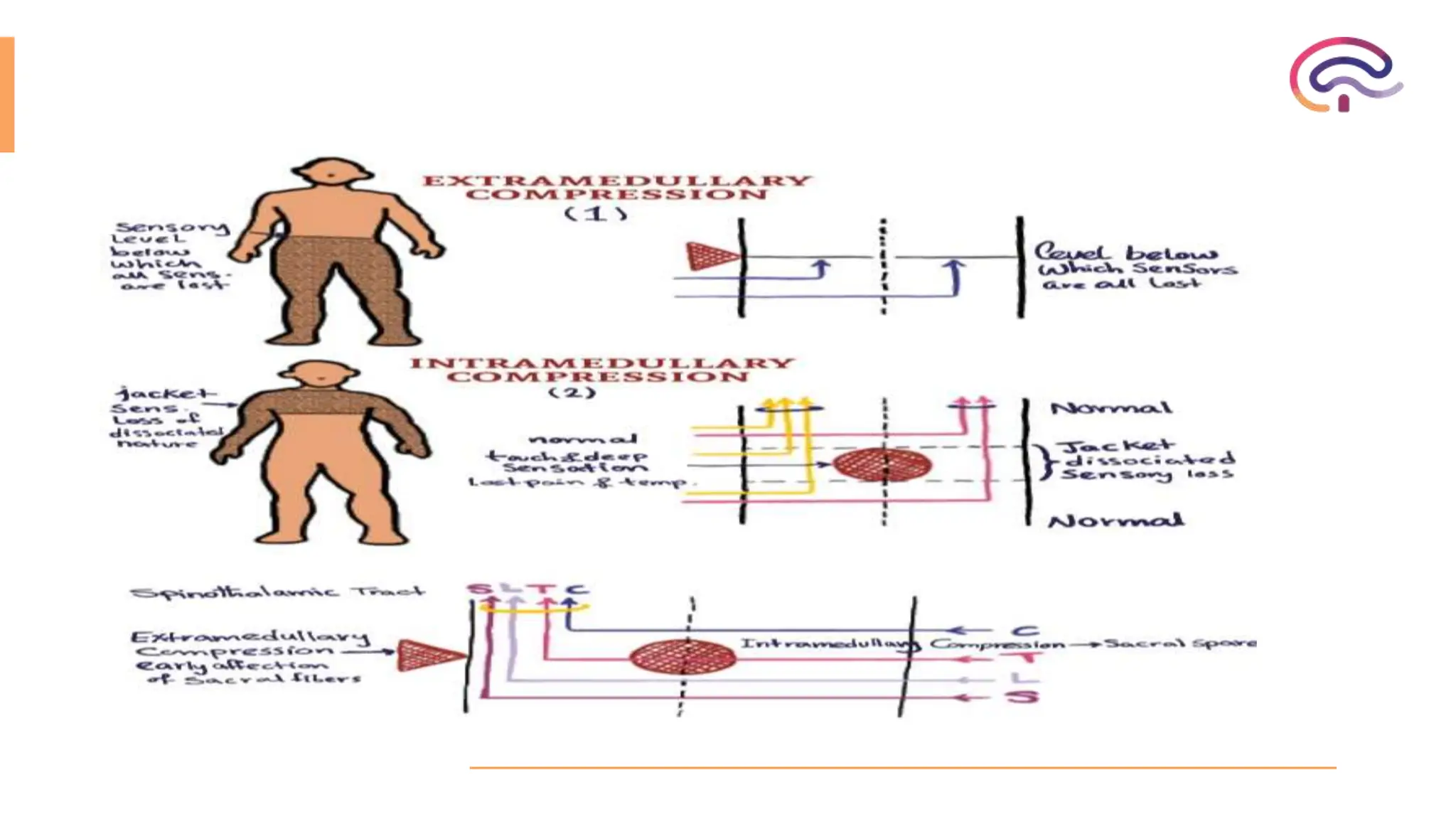
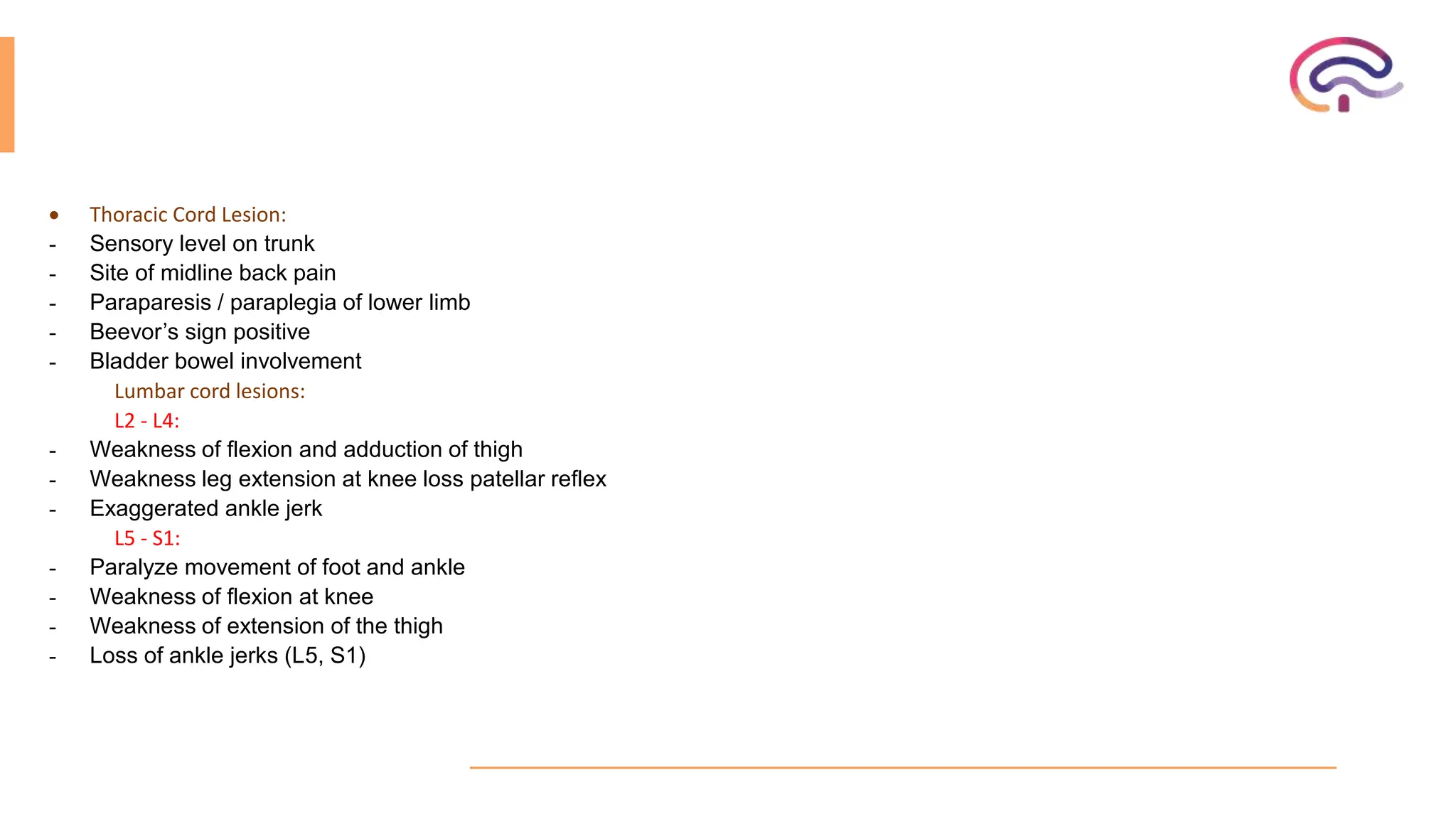
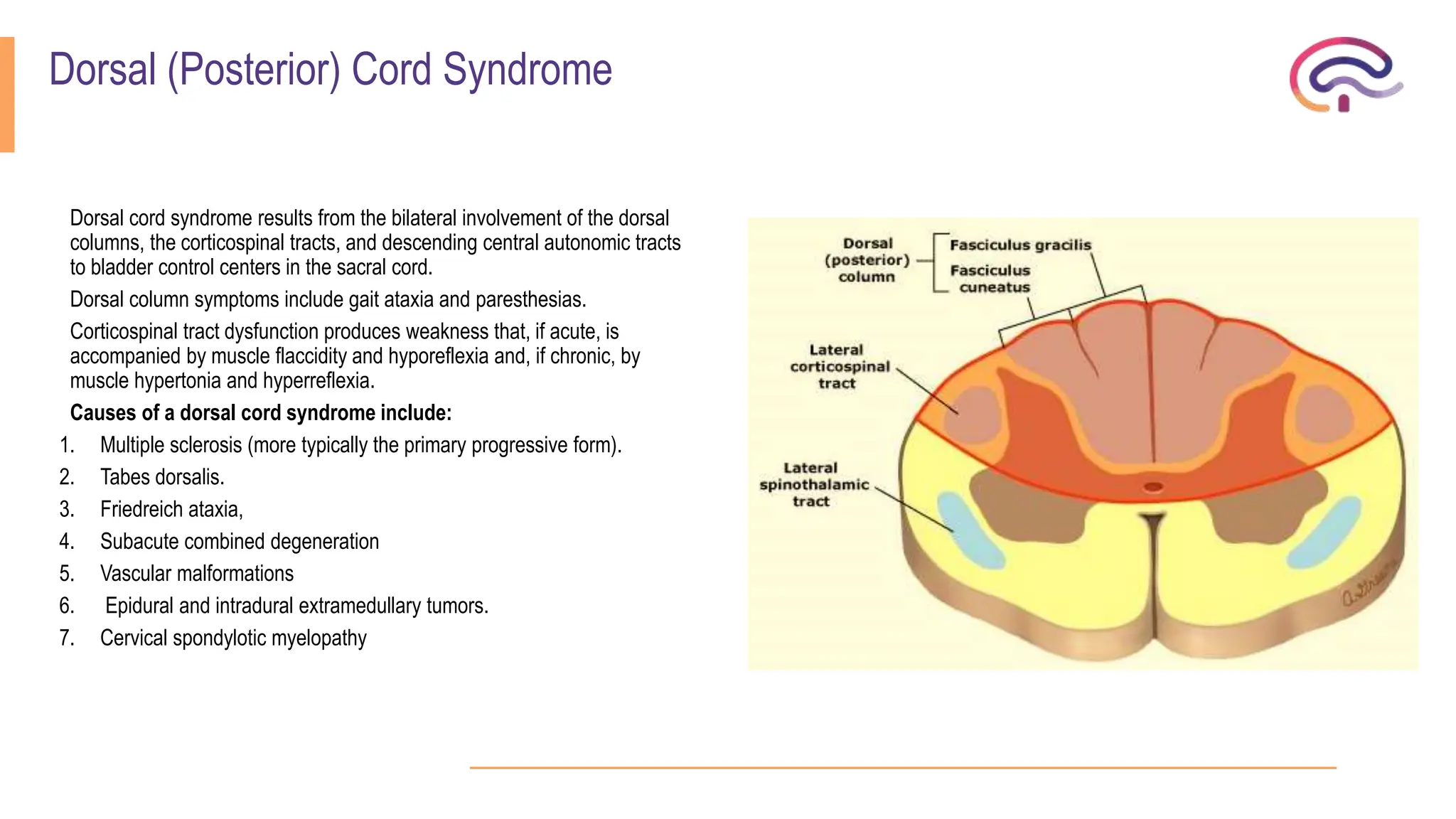
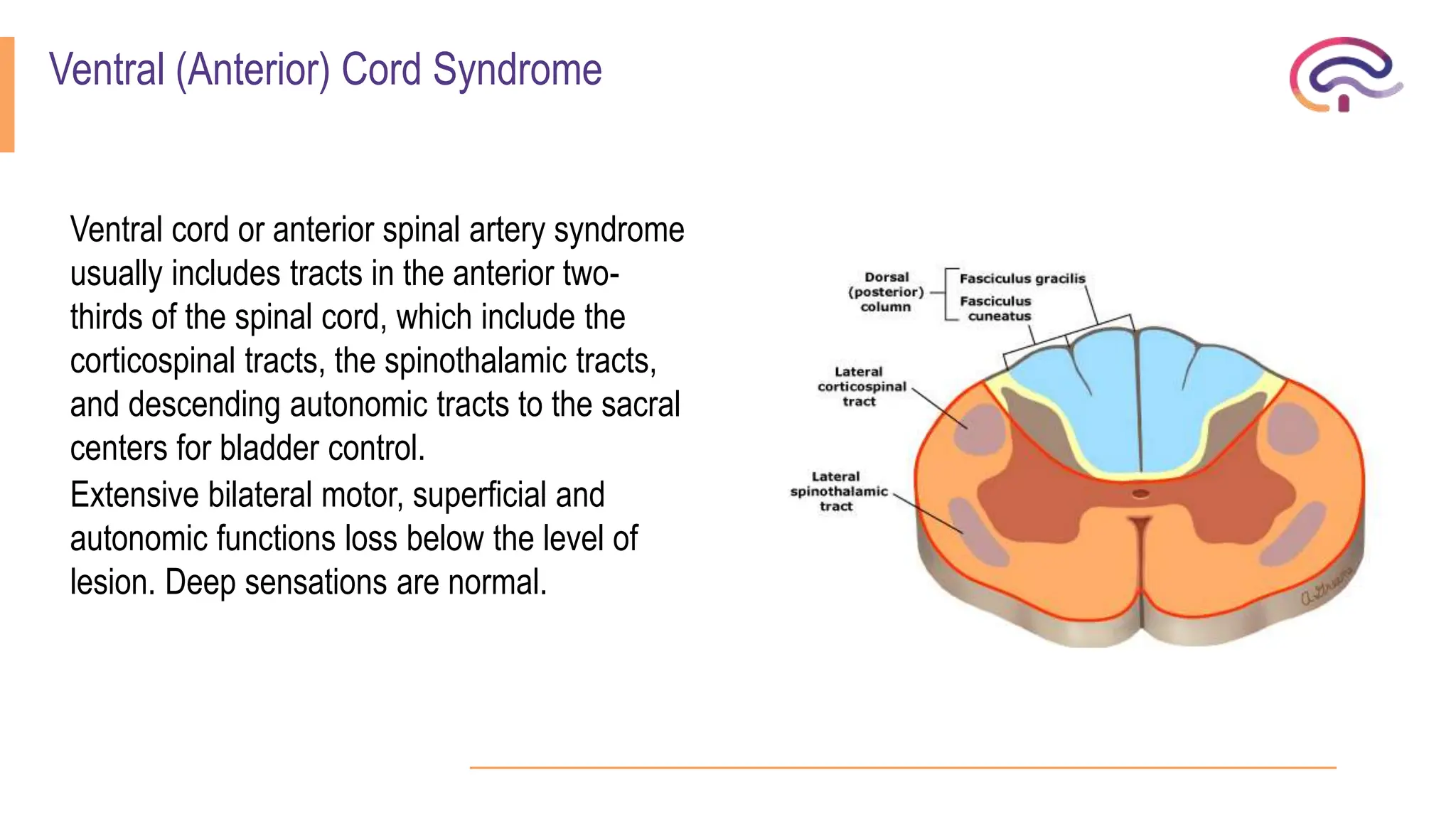
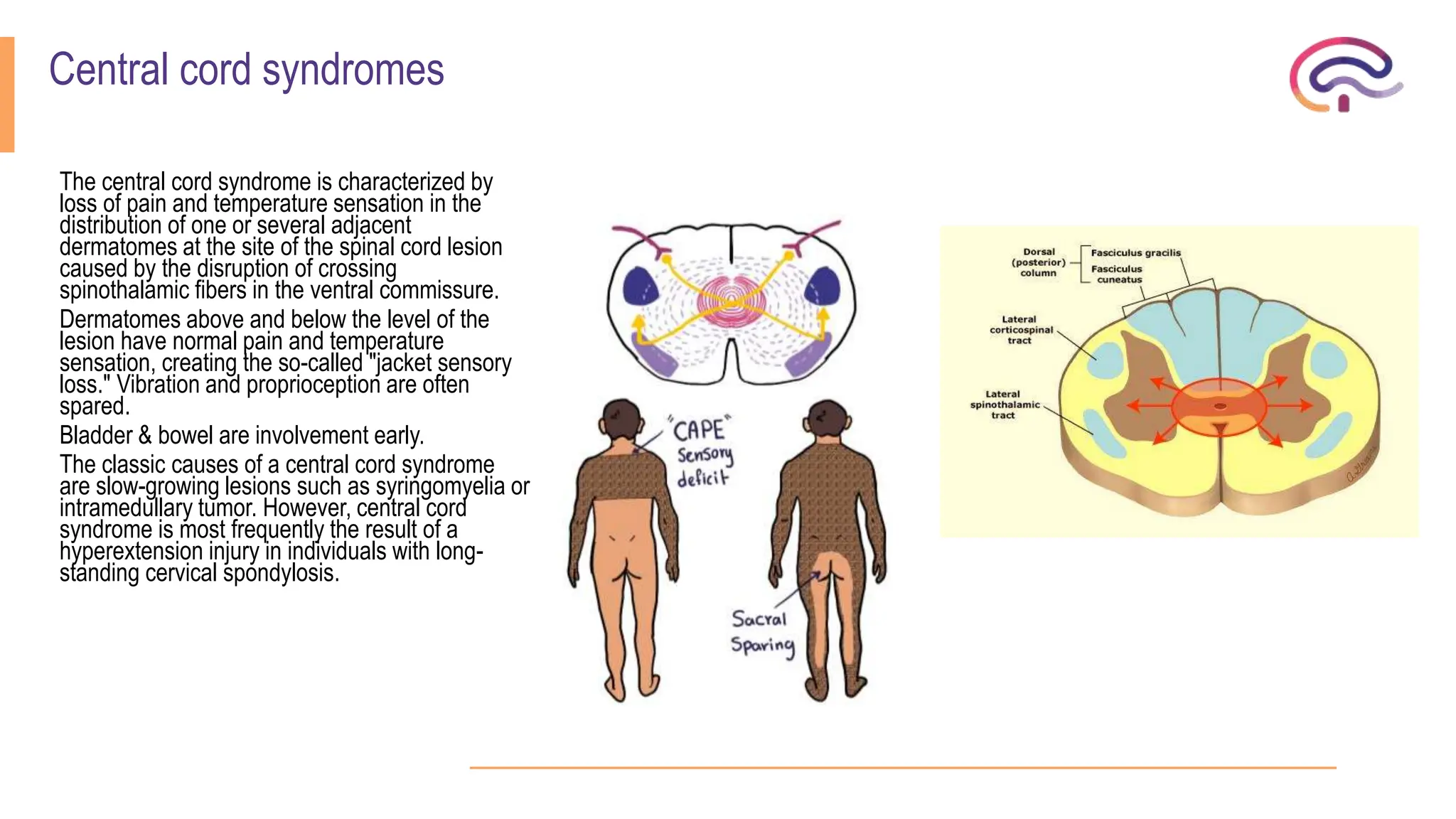
The document outlines various spinal cord disorders, including myelopathy, myelitis, and radiculopathy, explaining their causes, symptoms, and clinical manifestations. It also discusses paraplegia, detailing its types, causes, and the specific associated symptoms and diagnostic markers. Additionally, it covers segmental syndromes and provides information on different spinal cord syndromes, their characteristics, and significant clinical presentations.