Upper Respiratory Tract Infections: Pharyngitis, Epiglottitis, Deep Infections in Head and Neck
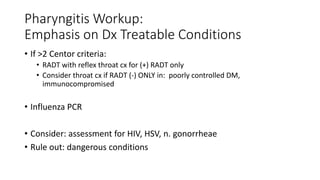
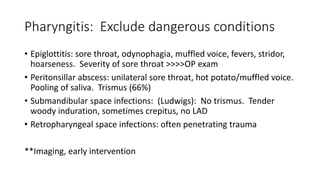
The document discusses various upper respiratory tract infections including pharyngitis, epiglottitis, and deep neck space infections. It provides guidelines for evaluating and diagnosing pharyngitis using the Centor criteria to determine if testing for Group A streptococcus is needed. It also discusses non-streptococcal causes of pharyngitis and outlines considerations and workup for dangerous deep neck space infections like epiglottitis and peritonsillar abscesses. The goal is to appropriately diagnose and treat conditions like streptococcal pharyngitis while excluding