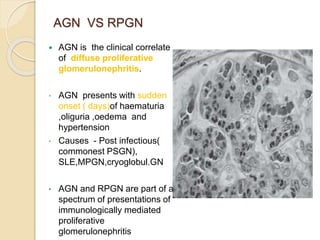
Glomerular diseases involve the glomeruli of the kidney and can lead to proteinuria and/or hematuria. They are classified based on clinical presentation, pathology, and renal biopsy findings. The most common presentations are nephrotic syndrome and nephritic syndrome. Nephrotic syndrome is characterized by proteinuria, hypoalbuminemia, edema, and hyperlipidemia. Nephritic syndrome presents with hematuria, hypertension, and reduced kidney function. Common causes include minimal change disease, membranous nephropathy, and focal segmental glomerulosclerosis.