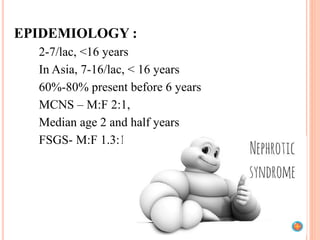
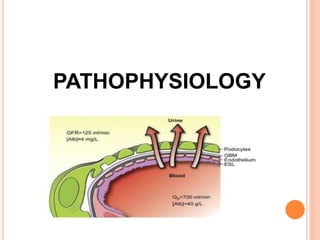
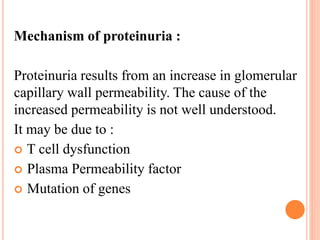
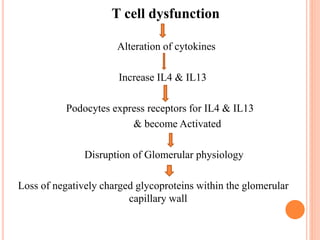
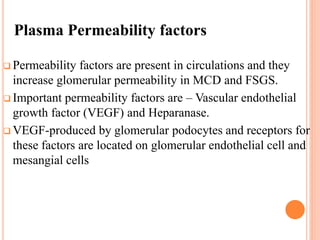
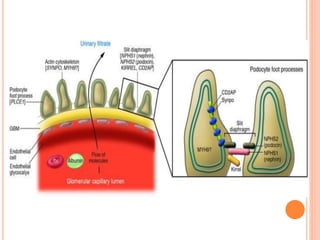
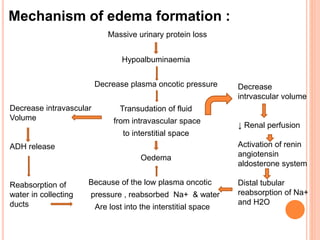
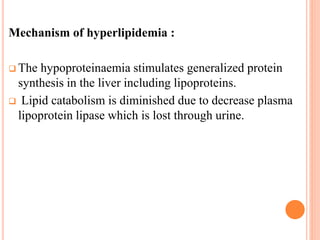
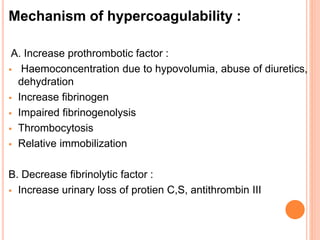
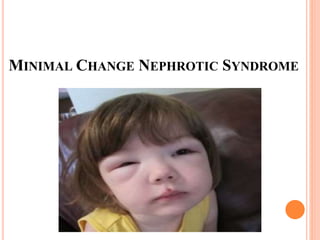
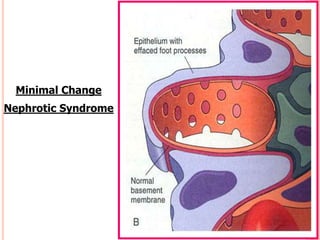
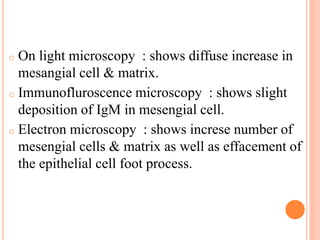
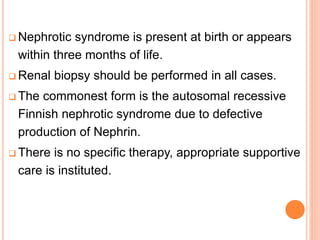
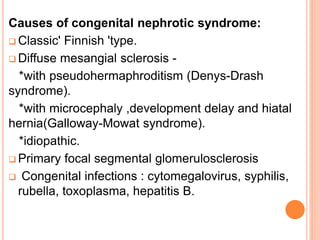
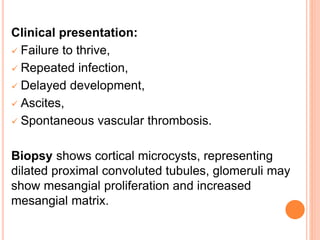
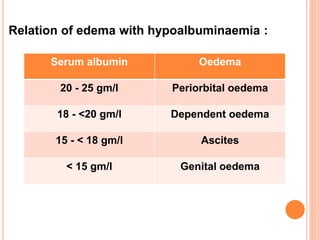
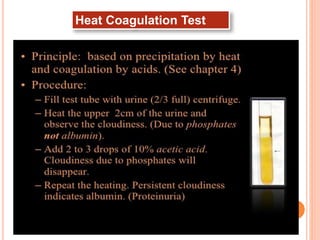
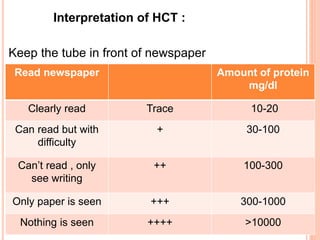
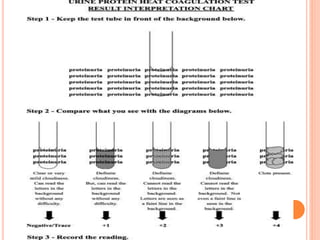
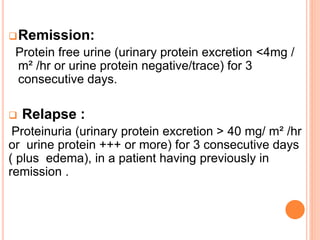
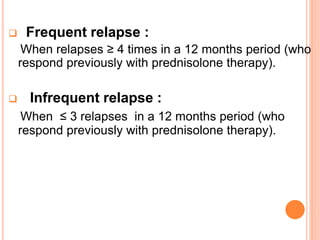
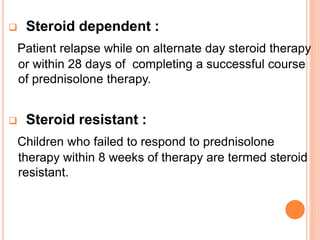
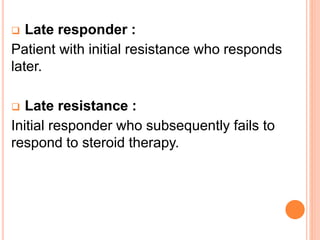
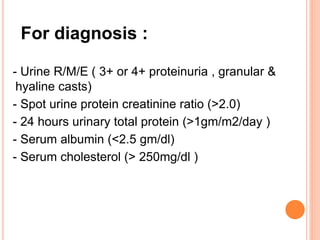
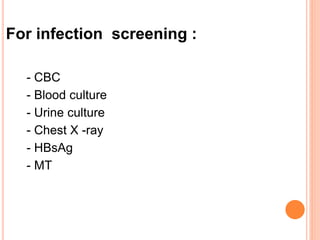
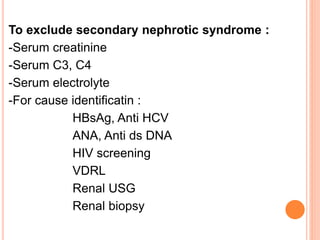
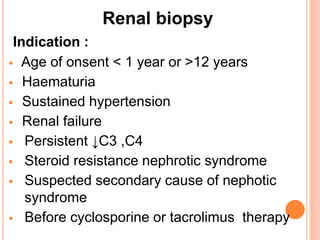
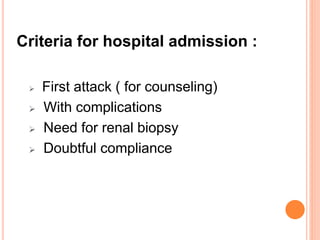
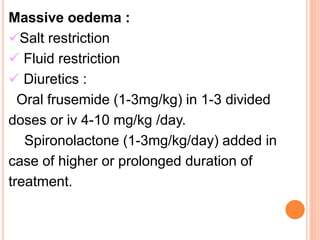
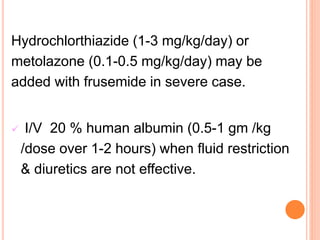
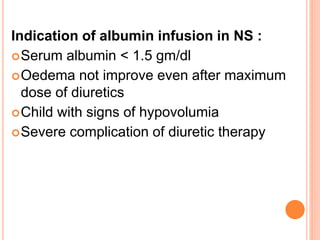
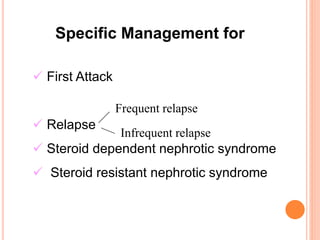
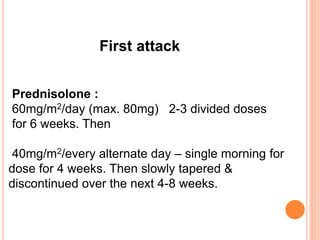
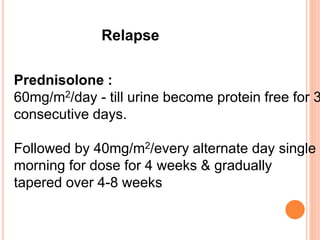
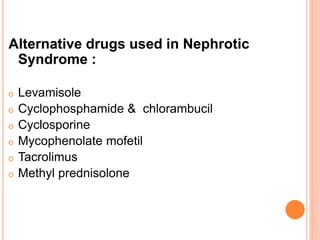
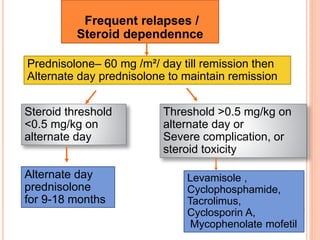
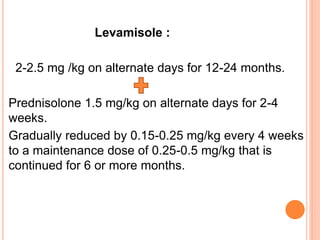
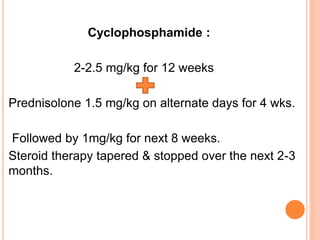
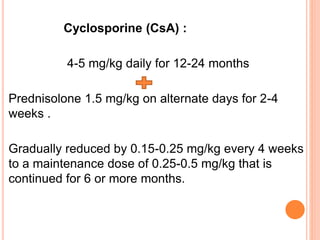
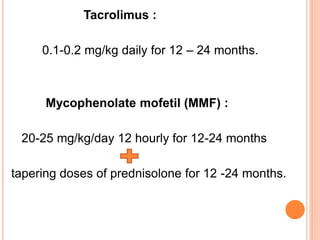
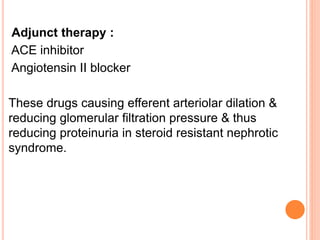
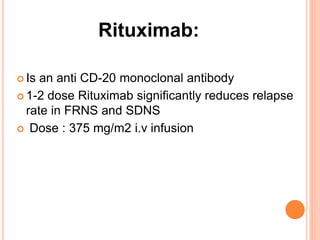
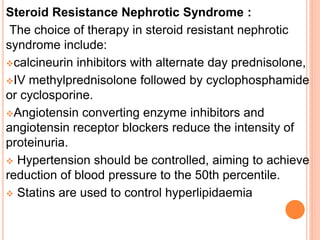
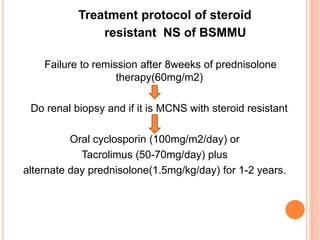
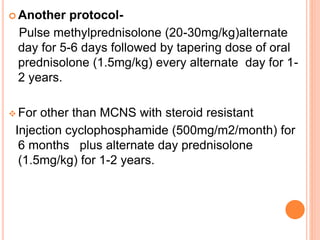
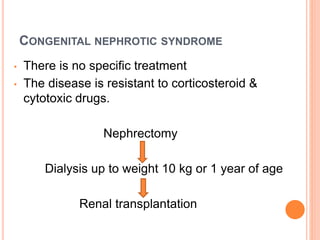
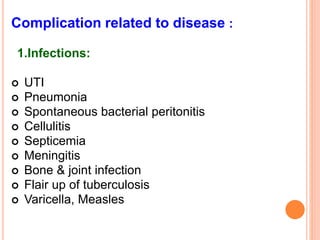
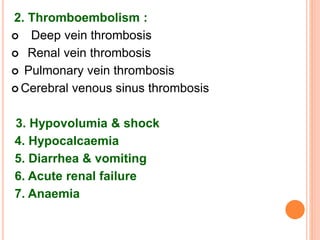
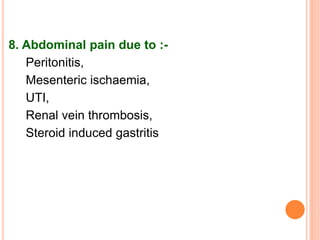
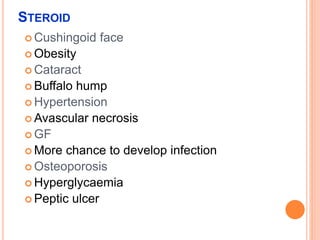
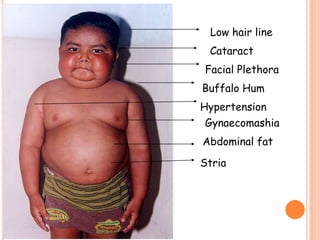
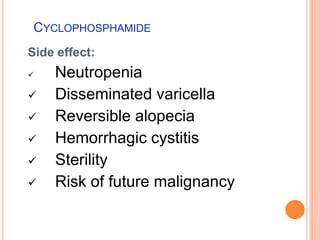
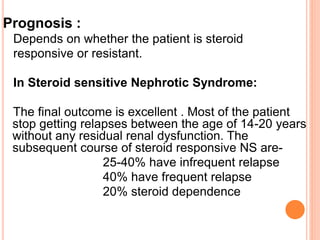
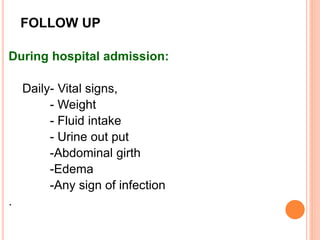
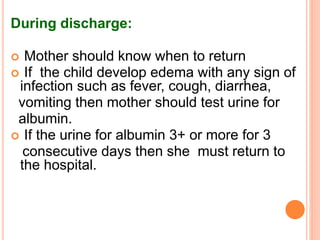
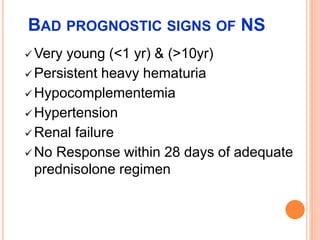
The document provides an overview of nephrotic syndrome, detailing its characteristics, epidemiology, pathophysiology, etiology, and types. It discusses the mechanisms of proteinuria, edema formation, hyperlipidemia, and hypercoagulability, as well as management strategies including dietary considerations, medication protocols, and complications associated with the condition. The content also outlines specific types of nephrotic syndrome such as minimal change nephrotic syndrome and focal segmental glomerulosclerosis, along with their clinical presentations and treatment approaches.