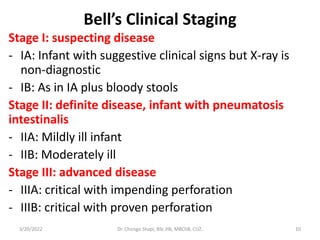
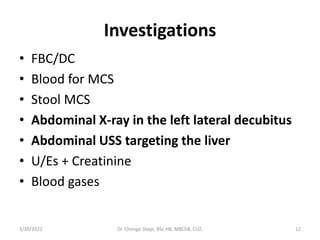
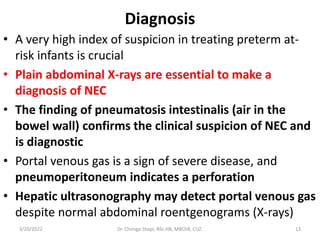
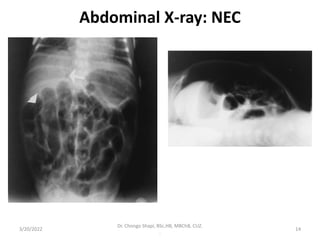
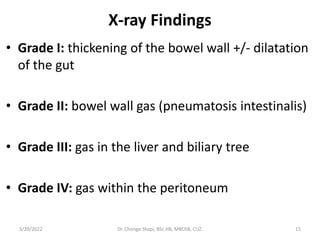
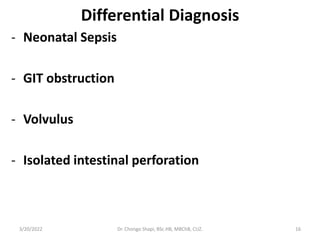
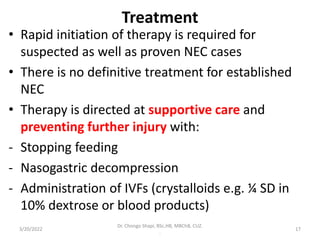
Neonatal necrotizing enterocolitis (NEC) is a serious gastrointestinal emergency primarily affecting preterm infants, characterized by intestinal necrosis and high mortality rates. Risk factors include prematurity, low birth weight, rapid feeding, and infections, with symptoms such as feeding intolerance and abdominal distension appearing shortly after birth. Diagnosis relies on clinical suspicion and imaging, while management involves supportive care, antibiotics, and potentially surgery for severe cases.