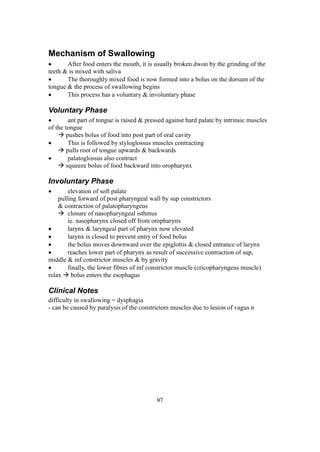
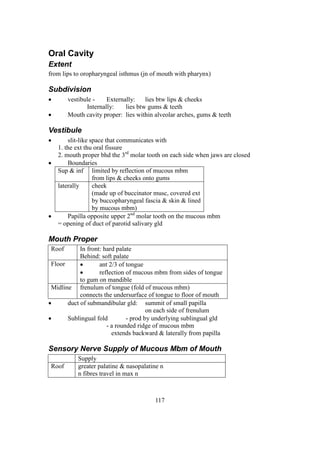
The document provides an extensive overview of human anatomy focused on the head and neck, detailing various muscles, arteries, nerves, and glands. It includes anatomical descriptions, relationships with surrounding structures, and clinical notes on conditions such as torticollis and thyroid disorders. Key topics covered are the sternocleidomastoid muscle, thyroid gland, carotid arteries, and the division of the neck into anterior and posterior triangles.