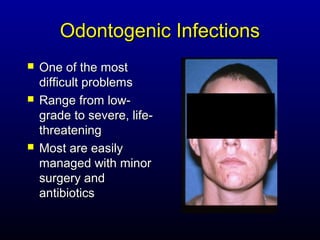
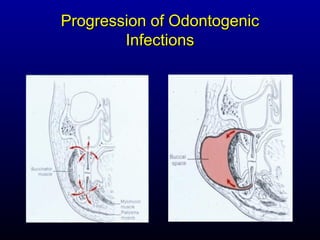
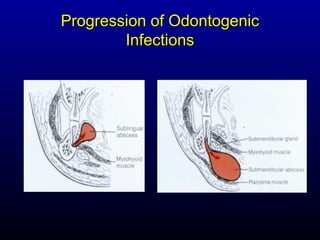
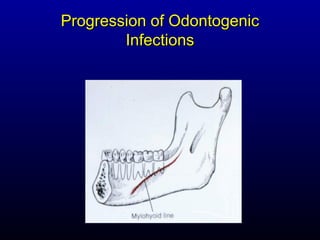
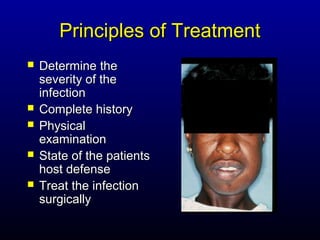
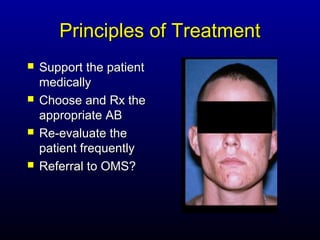
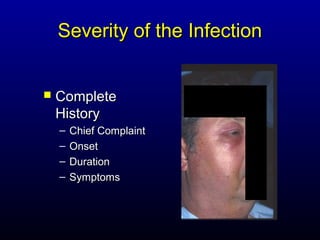
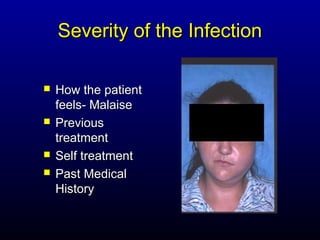
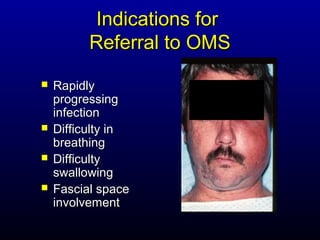
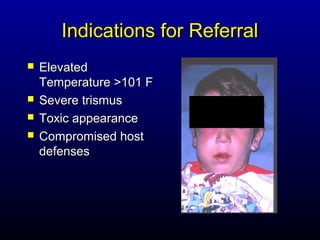
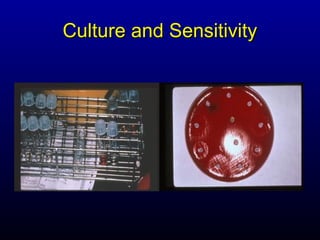
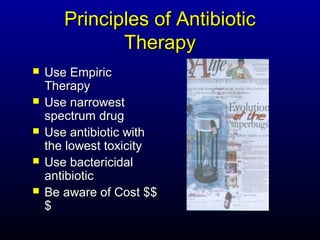
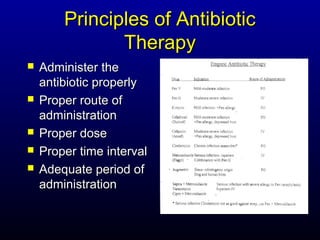
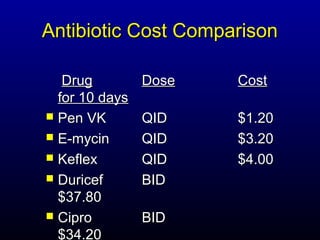
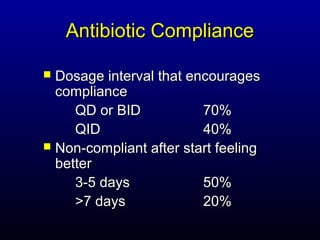
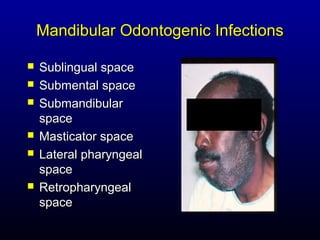
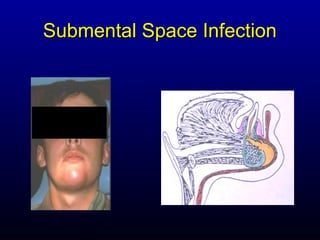
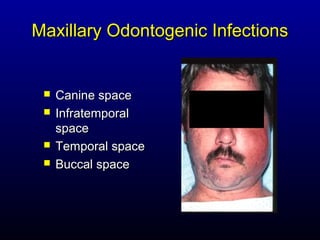
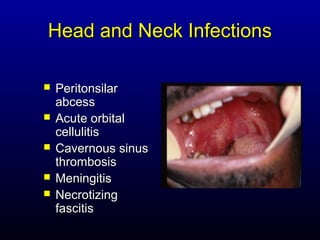
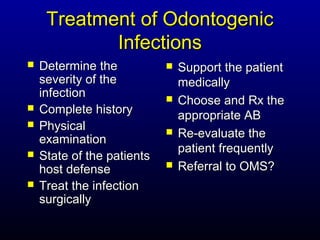
Odontogenic infections can range from minor to life-threatening. They are usually polymicrobial infections involving both aerobic and anaerobic bacteria from the normal oral flora. Infections may progress from periapical or periodontal sites to involve surrounding soft tissues or fascial spaces. Treatment involves determining the severity of infection, addressing the source surgically, prescribing appropriate antibiotics based on culture/sensitivity, and supporting the patient medically. More severe or progressive infections may require referral to an oral and maxillofacial surgeon.