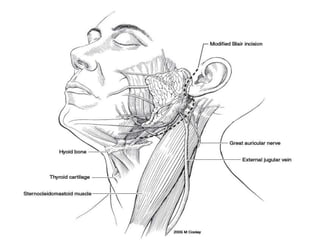
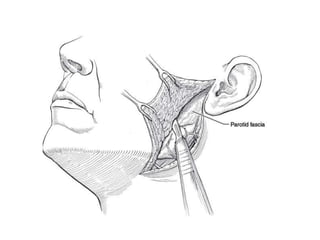
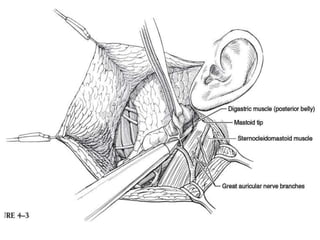
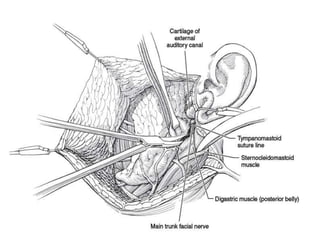
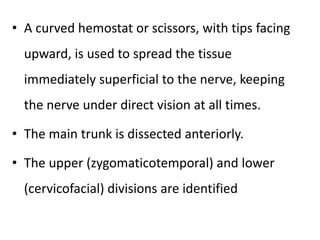
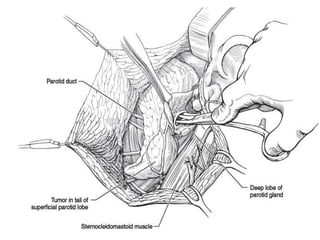
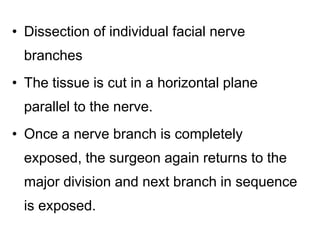
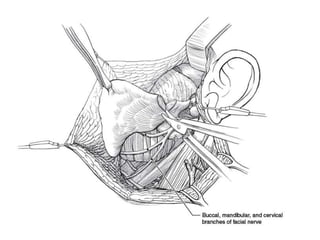
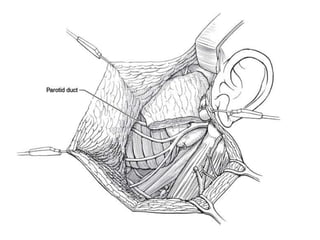
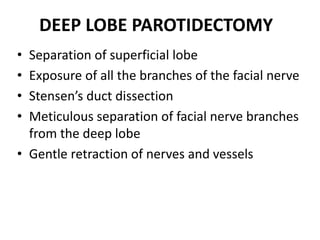
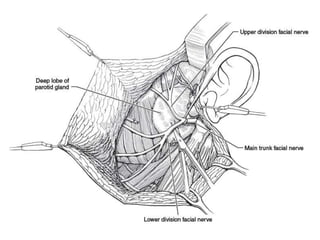
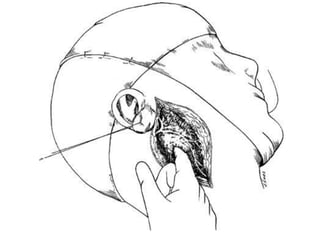
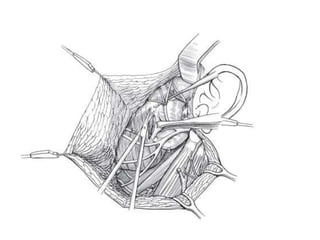
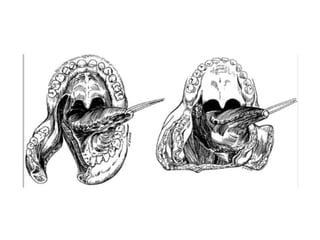
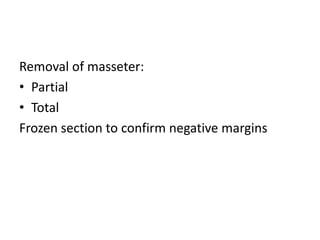
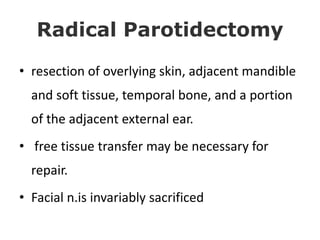
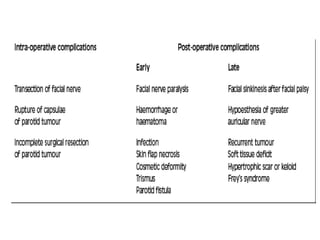
This document discusses the surgical procedures for parotid gland surgery. It describes the indications for superficial parotidectomy including benign tumors, refractory sialolithiasis, and chronic sialadenitis. The key anatomical landmarks are identified. The surgical techniques including patient positioning, incision, identification of the facial nerve branches, and approaches for superficial and deep lobe parotidectomy are outlined. Potential complications such as facial palsy, Frey's syndrome, and sialocele are discussed along with their management.