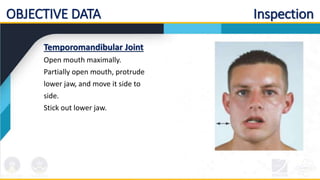
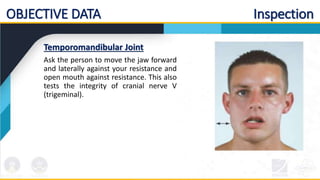
This document provides guidelines for conducting a physical examination of the musculoskeletal system. It outlines the standard protocol, including performing hand hygiene and explaining the procedure to the patient. It describes obtaining subjective information from the patient regarding joints, muscles, bones and functional assessment. It also lists the objective assessment steps including inspecting various areas like the temporomandibular joint, cervical spine, and shoulders while observing for any abnormalities.