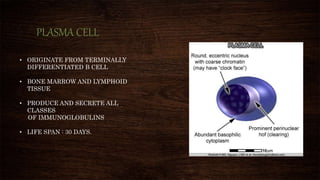
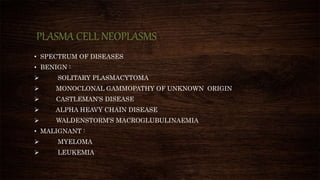
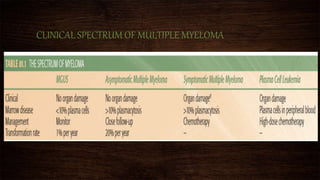
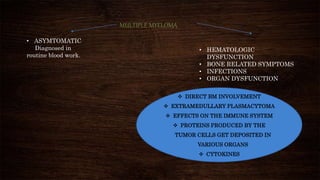
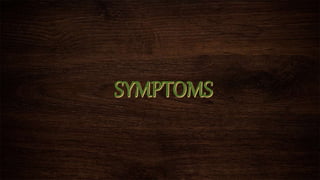
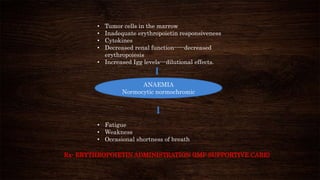
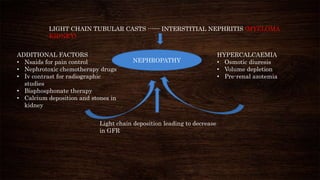
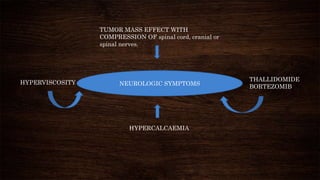
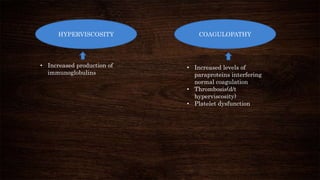
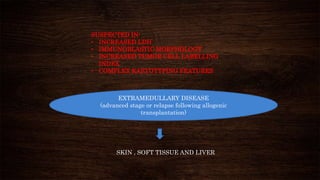
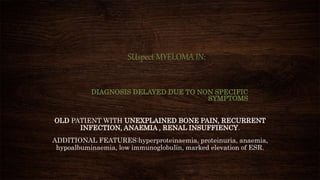
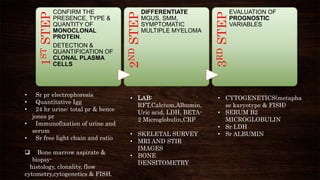
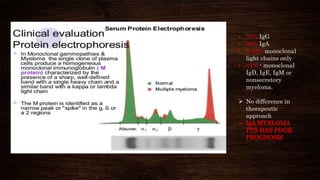
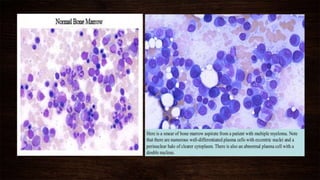
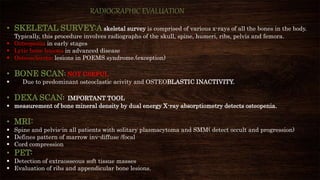
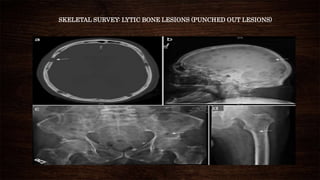
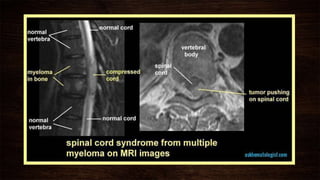
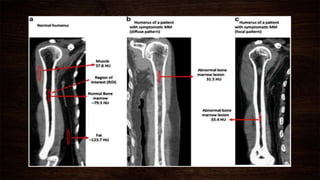
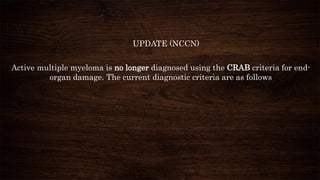
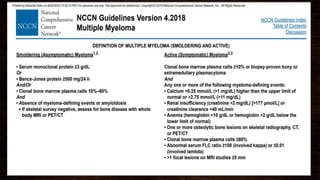
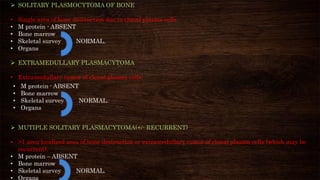
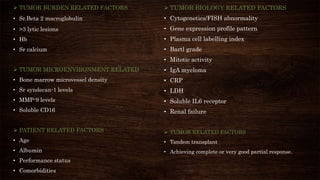
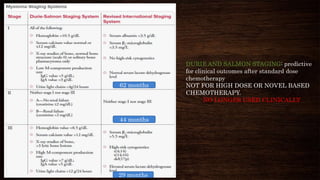
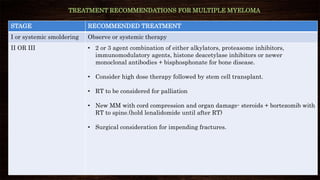
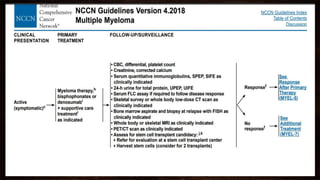
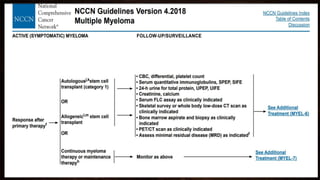
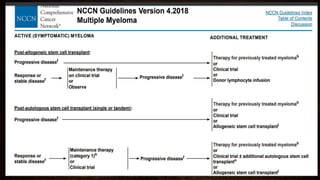
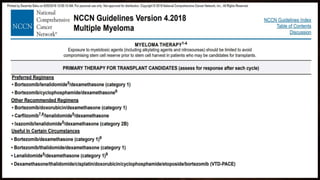
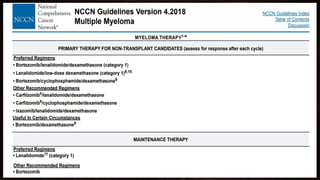
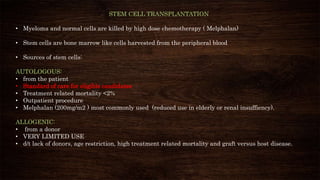
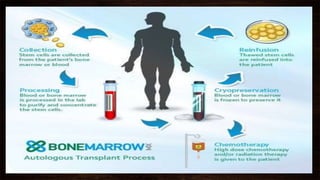
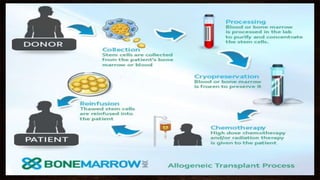
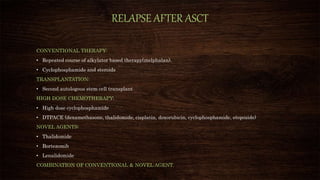
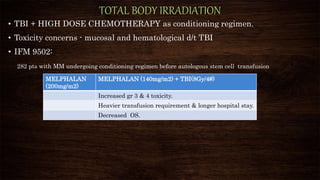
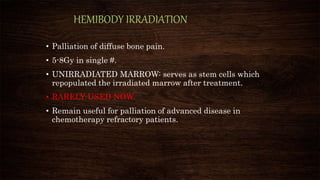
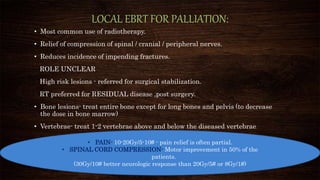
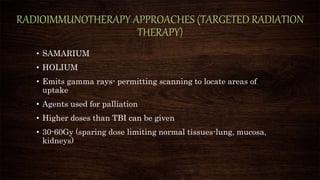
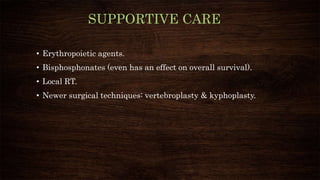
This document discusses multiple myeloma, a plasma cell neoplasm. It covers the epidemiology, etiology, clinical presentation, diagnostic workup, staging, prognostic factors, and treatment approaches for multiple myeloma. Key points include that multiple myeloma accounts for 22% of all mature B-cell neoplasms and presents with hematologic dysfunction, bone disease, infections, and organ impairment. Diagnosis involves blood and bone marrow tests to detect monoclonal proteins and clonal plasma cells. Treatment may include chemotherapy, stem cell transplantation, radiation therapy, immunotherapy, and management of symptoms.