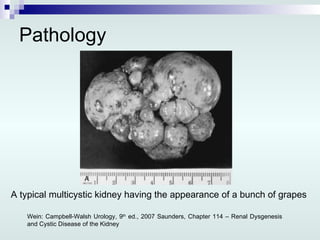
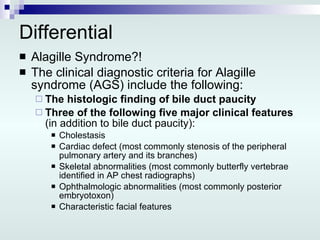
This document presents a case report of a newborn with multicystic dysplastic kidney (MCDK). The key points are:
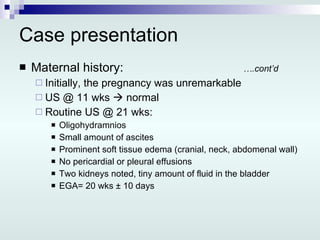
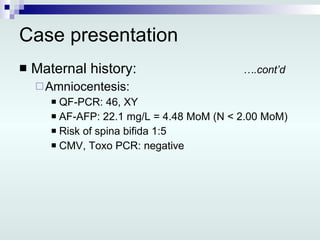
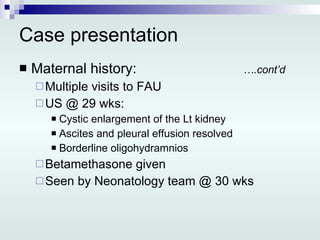
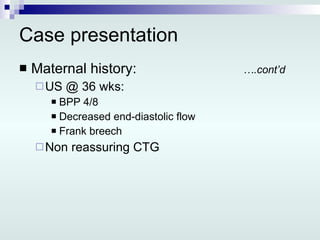
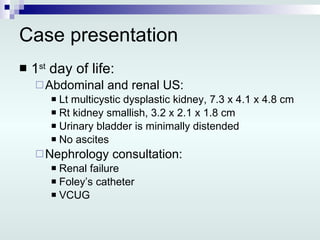
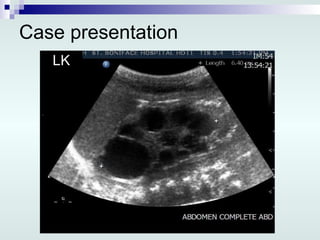
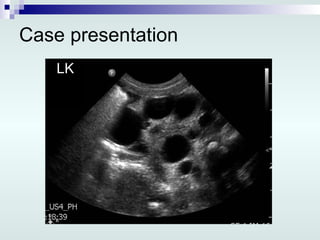
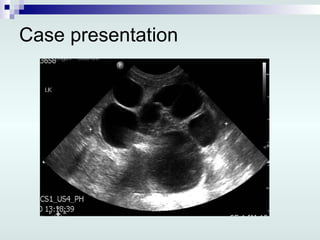
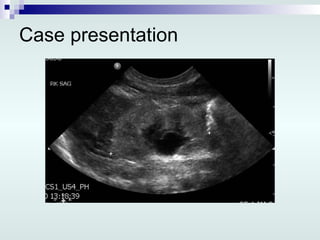
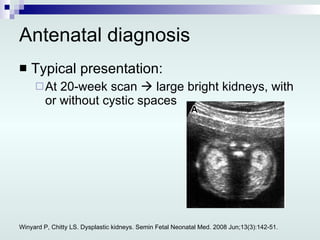
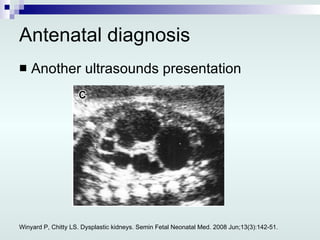
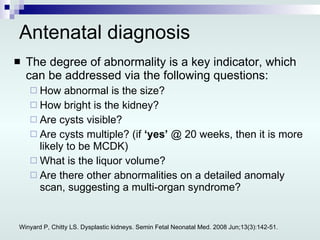
1) Prenatal ultrasound identified a cystic enlargement of the left kidney in the fetus.
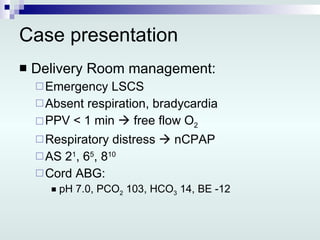
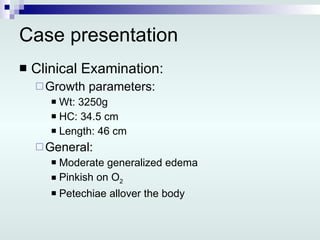
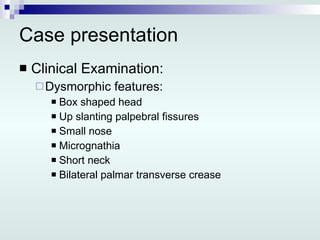
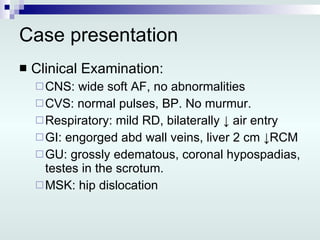
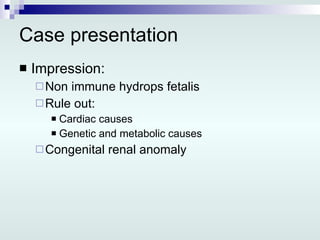
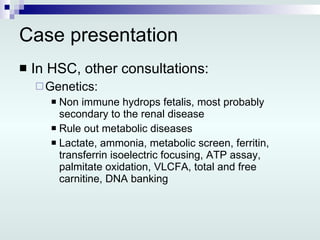
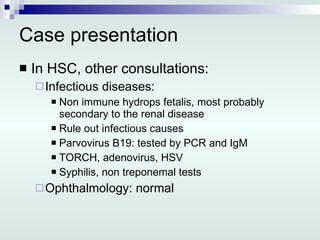
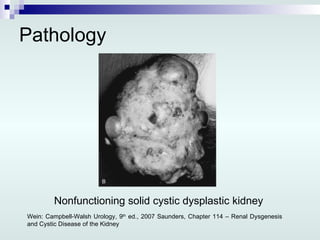
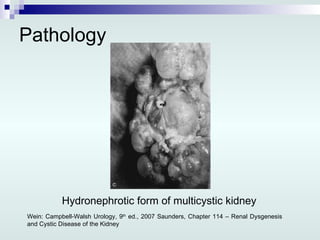
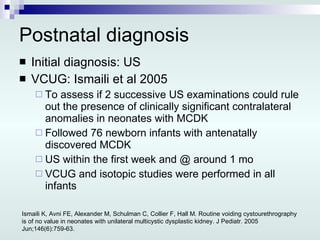
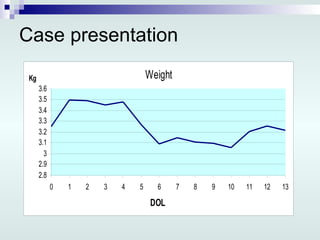
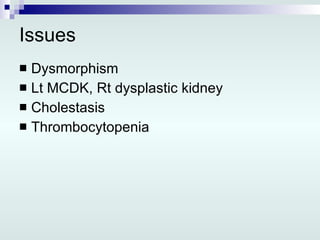
2) After a preterm delivery, examination of the newborn found generalized edema, dysmorphic features, and a grossly edematous left MCDK.
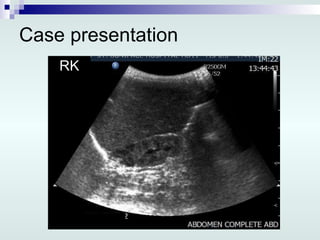
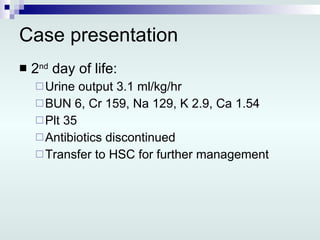
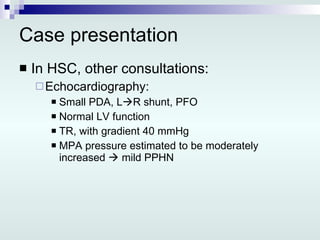
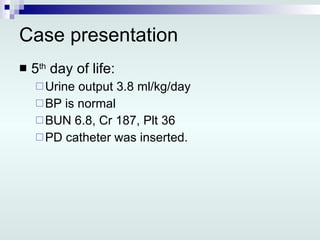
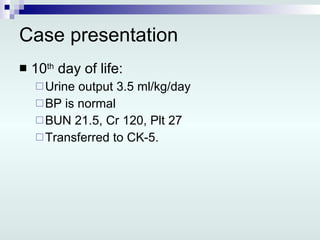
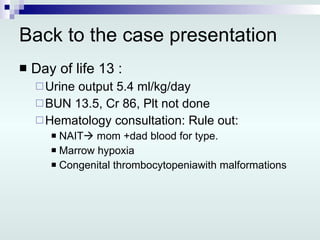
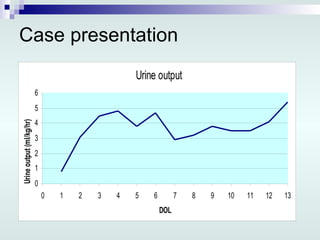
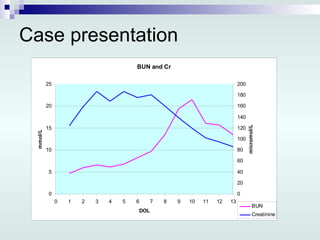
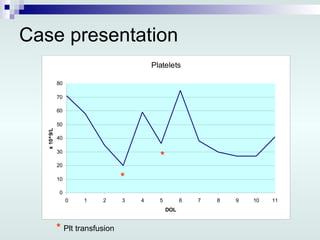
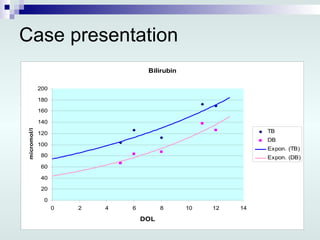
3) Workup revealed renal failure. Imaging showed a small right kidney. The newborn was treated with peritoneal dialysis.