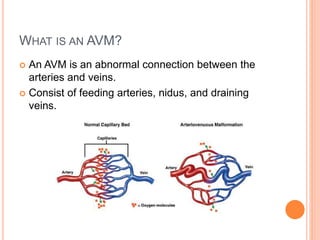
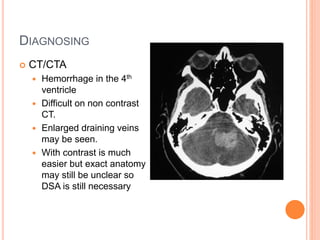
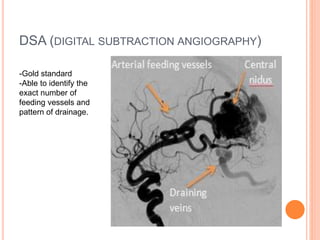
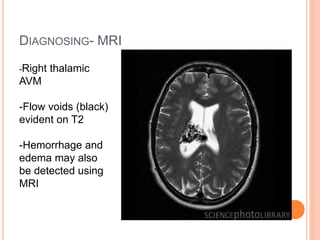
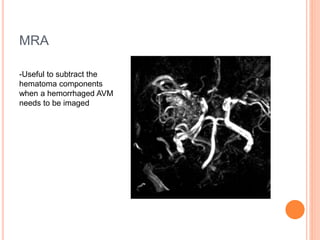
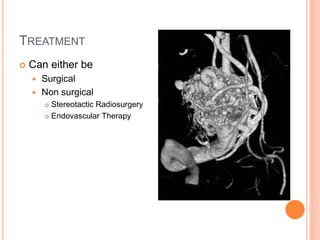
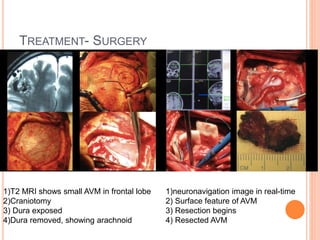
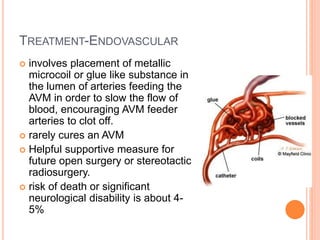
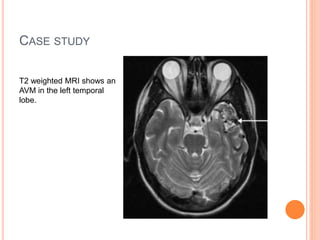
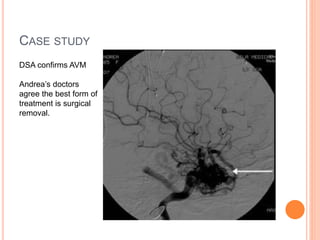
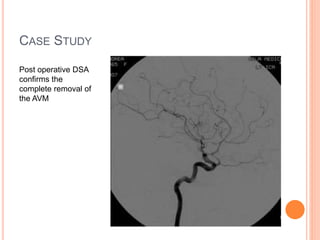
An AVM is an abnormal connection between arteries and veins that allows blood to bypass the capillary bed. AVMs can occur anywhere but are mostly found in the brain and spine. They may be asymptomatic or cause symptoms depending on their location and size. Diagnosis involves imaging tests like CT, MRI, MRA, and DSA. Treatment options include surgery, stereotactic radiosurgery, and endovascular embolization depending on the size, location, and risk profile of the AVM. Complete surgical removal remains the gold standard treatment for lower risk AVMs to eliminate the risk of hemorrhage.