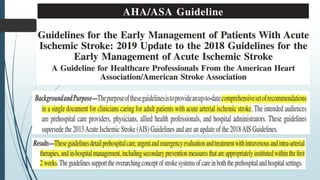
1. Regional stroke centers should be established to provide thrombolysis and transport to endovascular treatment centers. Every hospital should have a stroke team and protocols for emergency evaluation.
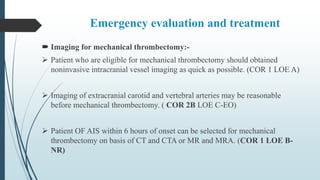
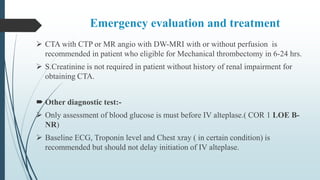
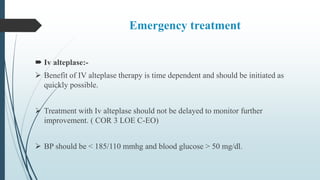
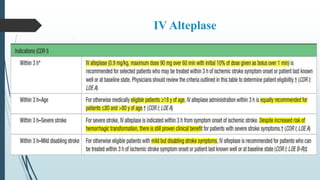
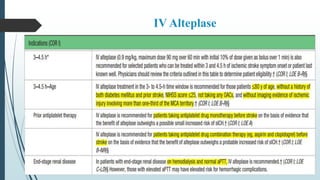
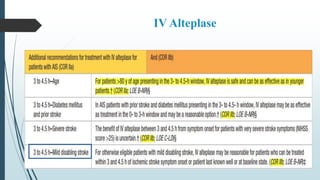
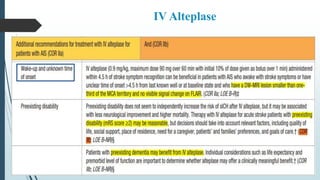
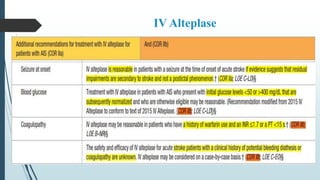
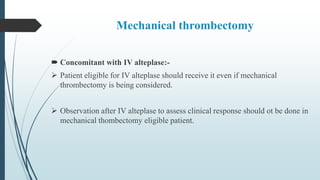
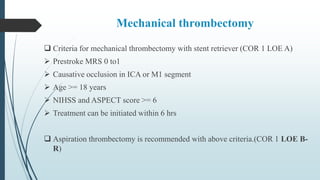
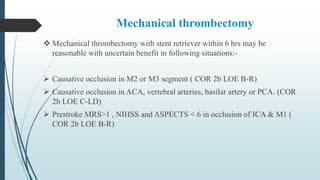
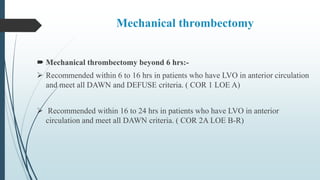
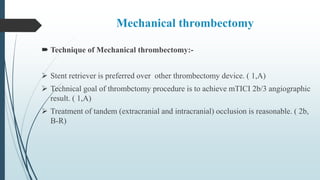
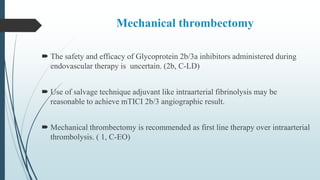
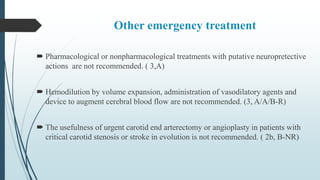
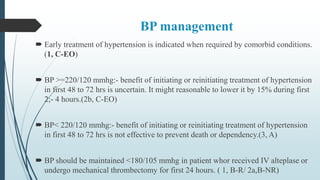
2. Patients should receive IV alteplase as quickly as possible if eligible. Mechanical thrombectomy is recommended for large vessel occlusions within 6-24 hours of onset depending on criteria.
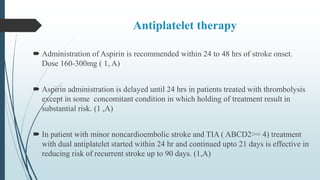
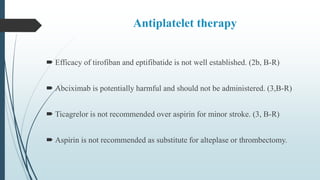
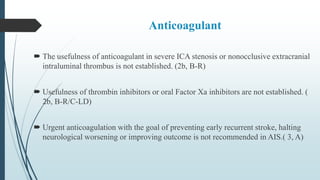
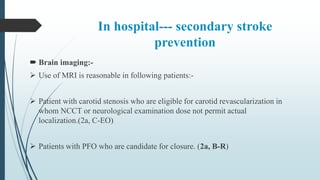
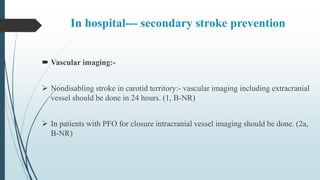
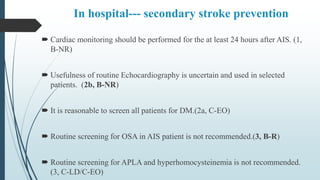
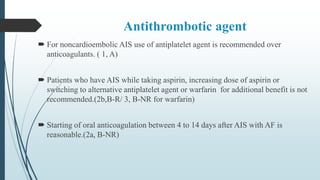
3. In-hospital prevention includes antiplatelet therapy, vascular imaging, and lipid management with statins to reduce cardiovascular risk.