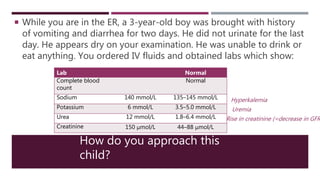
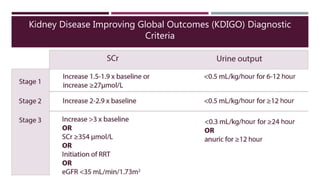
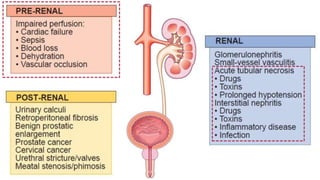
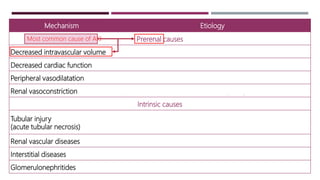
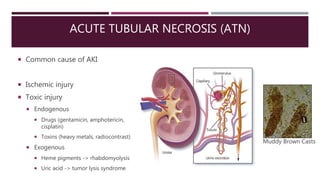
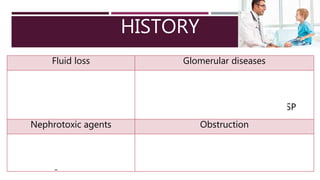
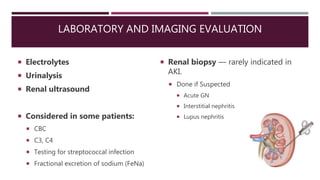
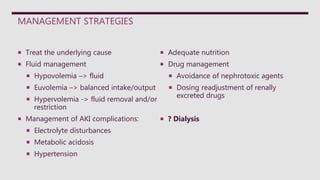
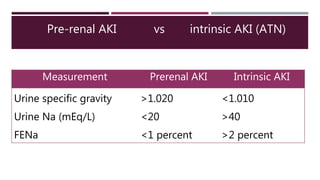
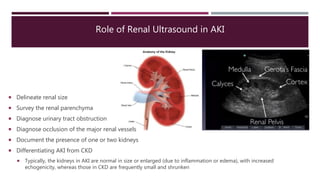
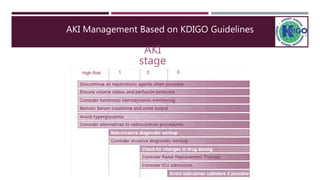
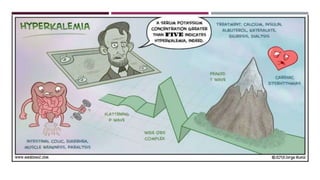
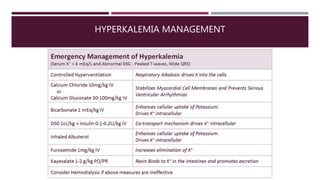
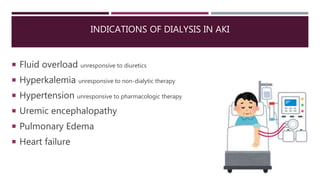
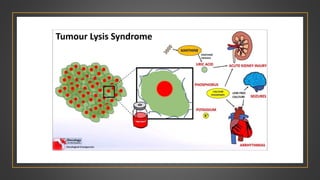
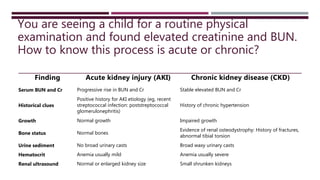
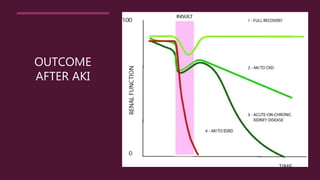
This document discusses acute renal failure in children. It begins by describing a case of a 3-year-old boy presenting with vomiting, diarrhea, and inability to urinate who is found to have hyperkalemia, uremia, and a rise in creatinine, indicating acute kidney injury. It then defines acute kidney injury and differentiates it from acute renal failure. It reviews causes of acute kidney injury including pre-renal, intrinsic renal from vascular, tubular, glomerular or interstitial issues, and post-renal obstruction. Evaluation, management focusing on treating the underlying cause and complications, and outcomes are discussed.