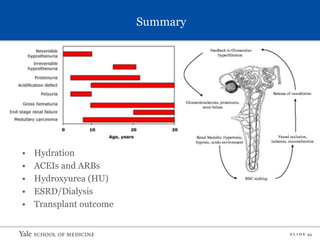
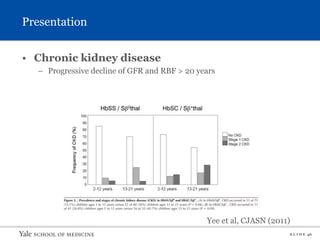
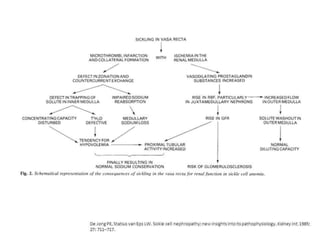
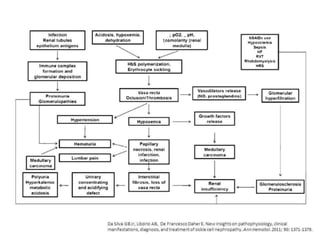
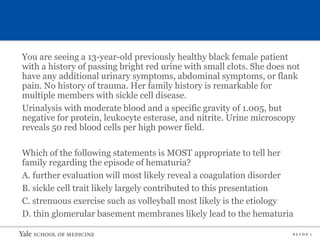
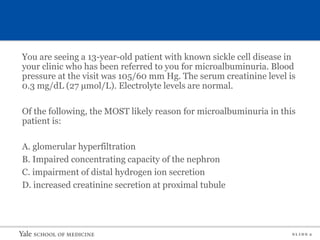
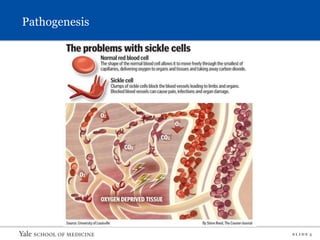
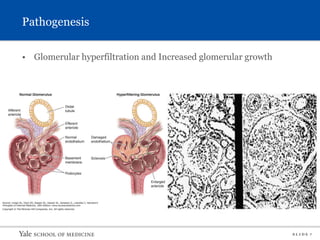
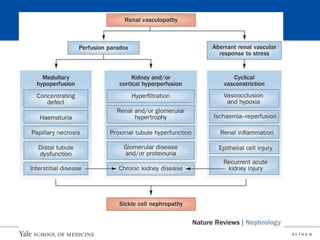
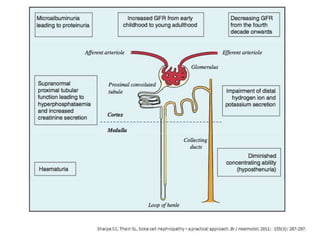
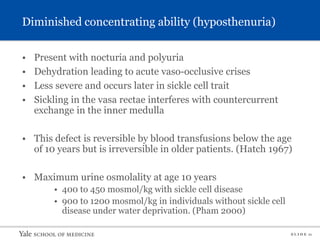
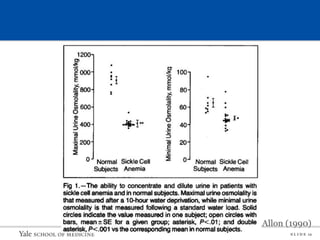
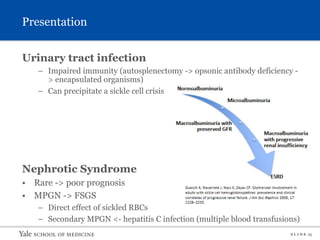
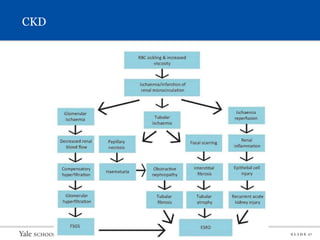
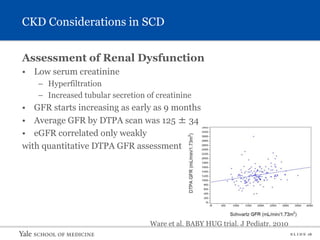
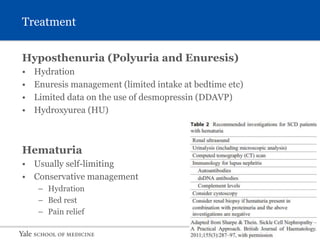
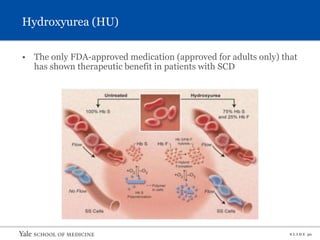
This document provides an overview of sickle cell nephropathy through slides presented in a lecture. It covers the epidemiology, pathogenesis, clinical presentation, diagnosis, treatment and management of chronic kidney disease for patients with sickle cell disease. Key points include that sickle cell nephropathy is caused by medullary hypoxia leading to tubulointerstitial disease and glomerular hyperfiltration. Common manifestations include hematuria, renal tubular acidosis, proteinuria, hypertension and chronic kidney disease. Treatment involves hydration, pain management, angiotensin converting enzyme inhibitors, hydroxyurea and blood transfusions in some cases.



![S L I D E 39
Future directions
More data!
The use of early detection biomarkers
• Early sickle cell nephropathy (eg, urinary endothelin 1 [ET-1],
neutrophil gelatinase-associated lipocalin (NGAL), and urinary
transforming growth factor (TGF) beta 1)
Bone marrow transplant effect on SCN](https://image.slidesharecdn.com/sicklecellnephropathy-220825172427-989b6365/85/Sickle-Cell-Nephropathy-pptx-40-320.jpg)