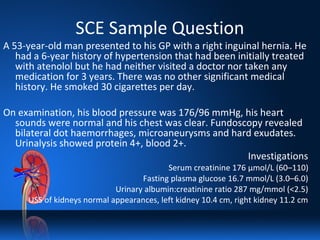
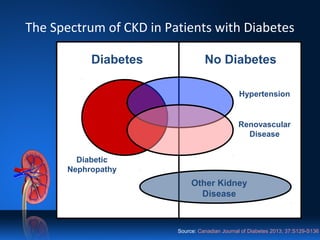
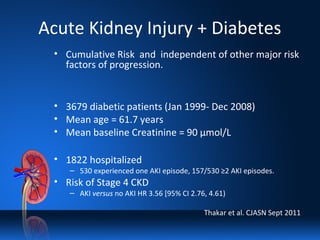
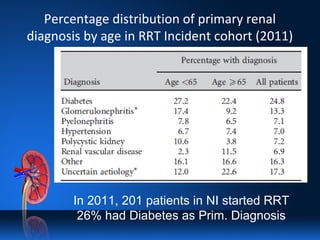
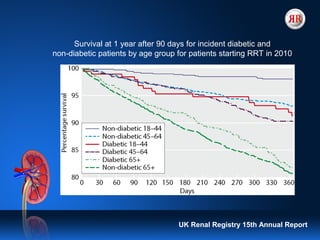
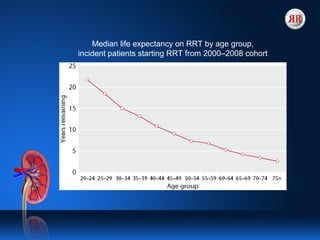
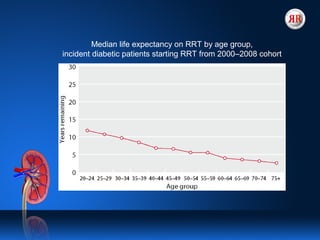
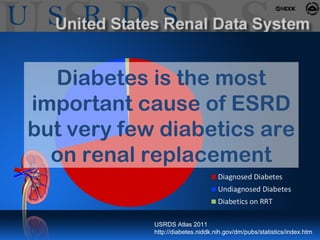
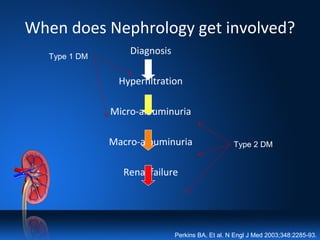
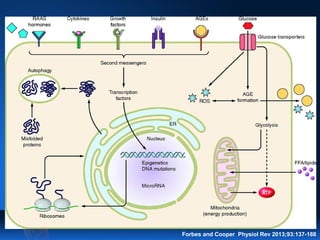
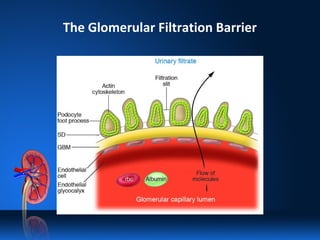
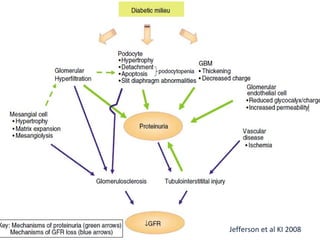
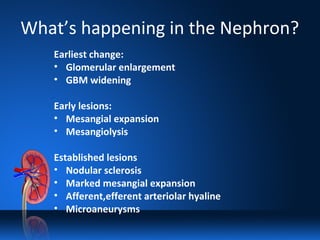
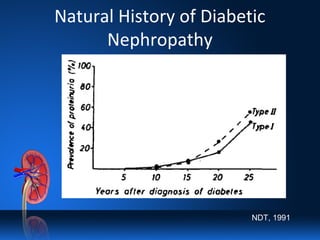
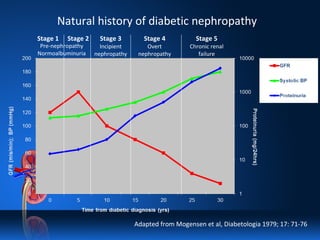
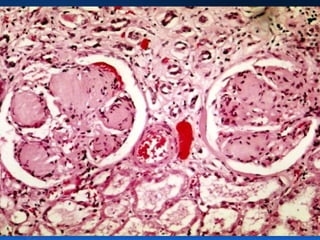
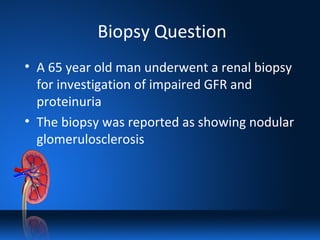
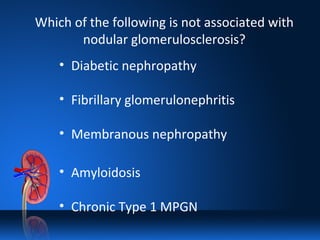
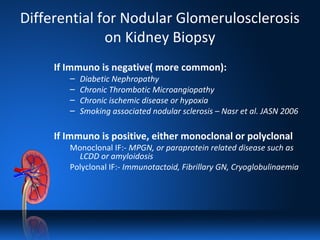
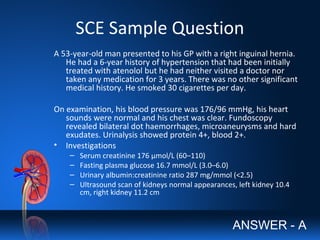
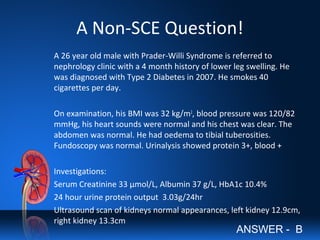
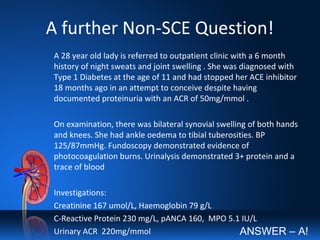
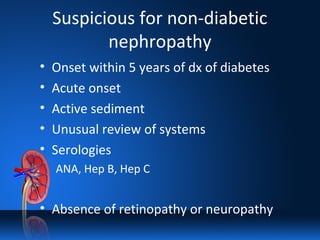
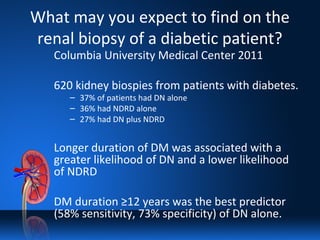
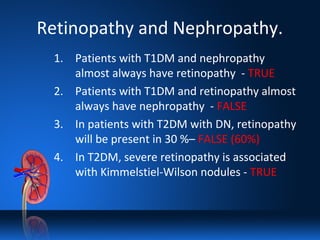
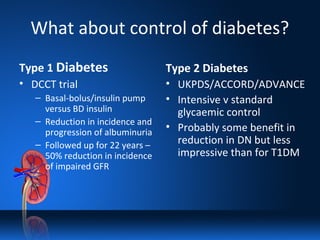
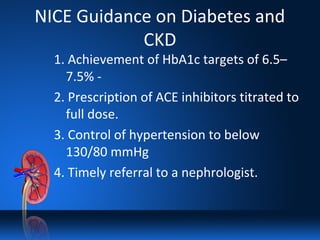
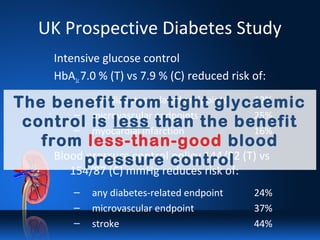
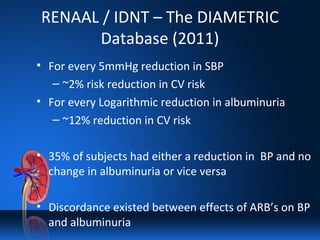
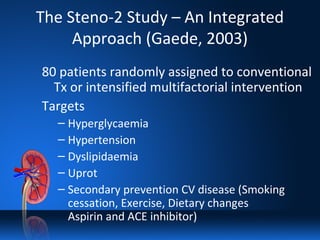
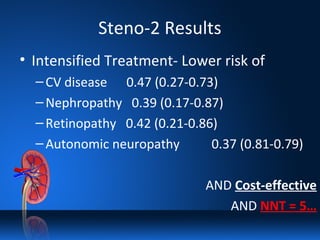
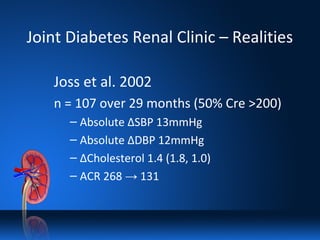
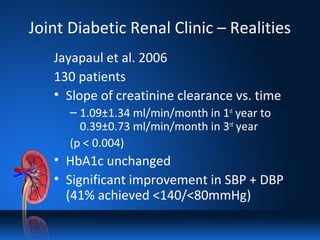
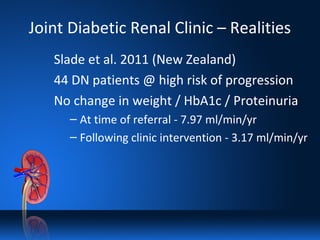
The document covers diabetic kidney disease, detailing its prevalence, impact, and pathogenesis, along with treatment strategies for managing diabetic nephropathy. It presents case studies and statistics to highlight the correlation between diabetes and chronic kidney disease, emphasizing the importance of integrated approaches in treatment. The document concludes that controlling blood pressure and proteinuria may provide greater benefits than glycemic control alone in managing diabetic nephropathy.