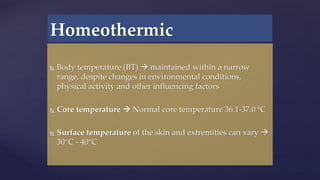
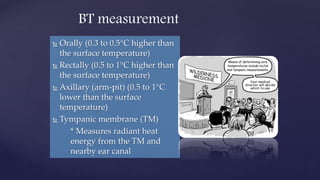
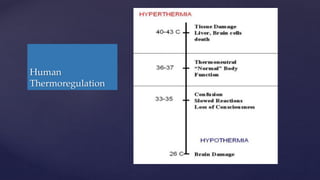
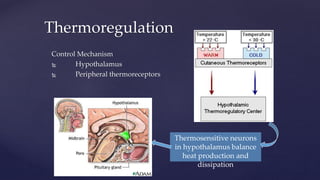
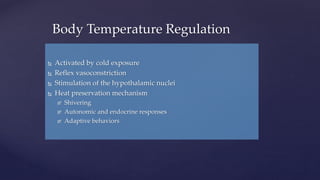
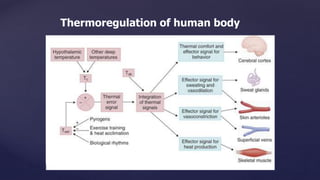
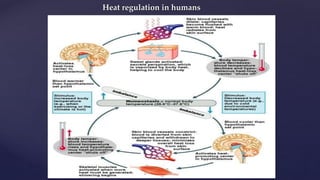
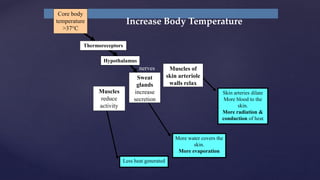
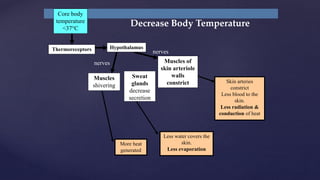
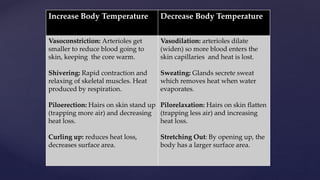
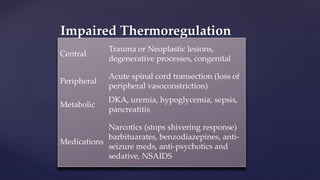
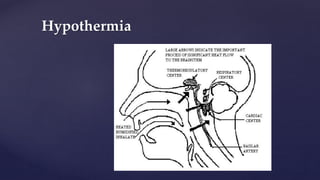
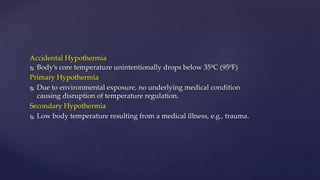
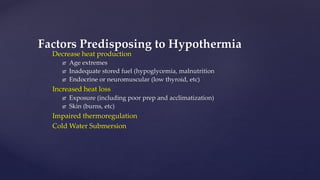
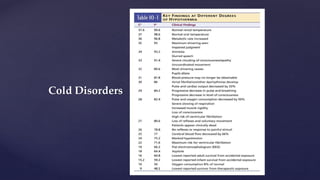
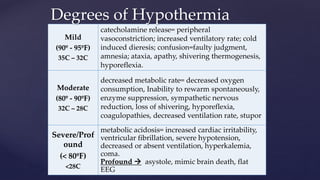
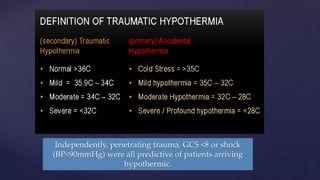
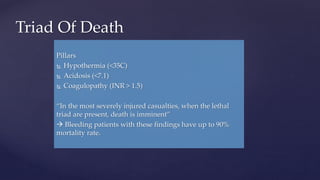
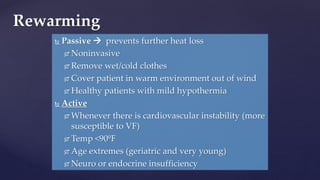
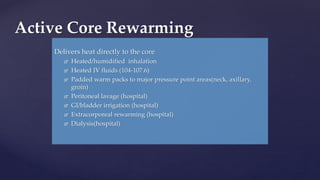
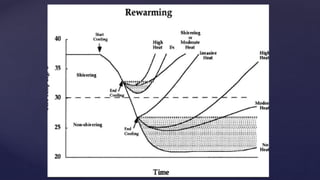
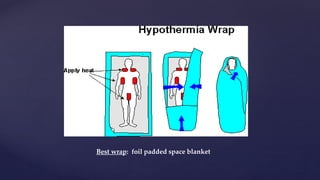
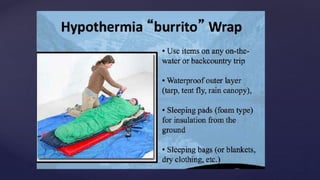
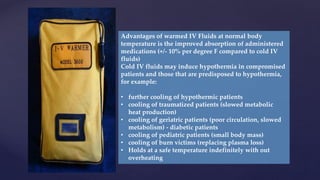
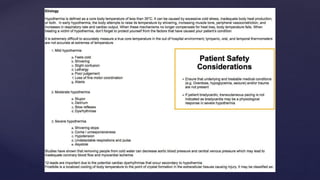
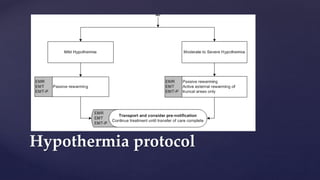
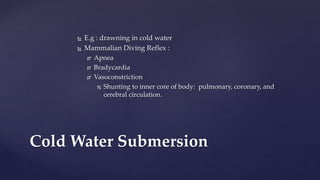
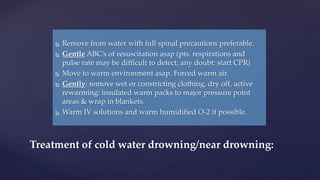
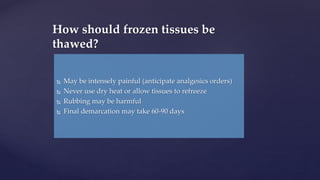
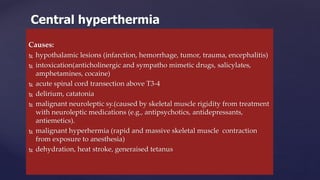
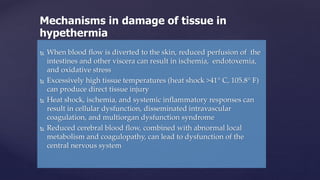
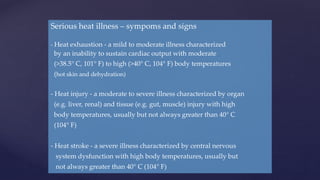
The document discusses human thermoregulation and metabolism. It describes how the hypothalamus controls thermoregulation through peripheral thermoreceptors to maintain core body temperature within a narrow range. It outlines the mechanisms used to increase or decrease body temperature, such as vasoconstriction/vasodilation, shivering, and sweating. Disorders like hypothermia and hyperthermia are also examined, along with their causes, symptoms, and treatment approaches.