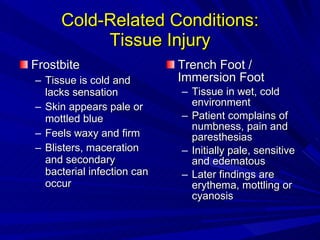
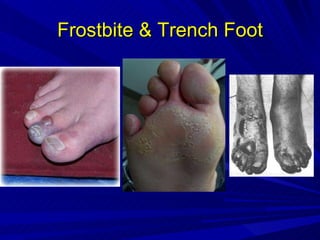
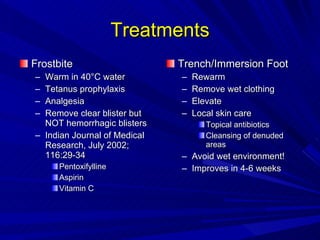
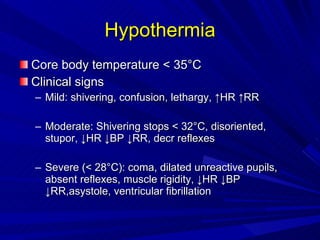
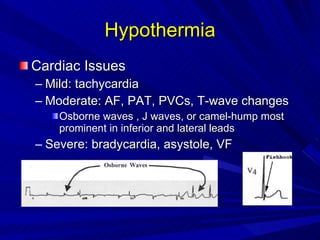
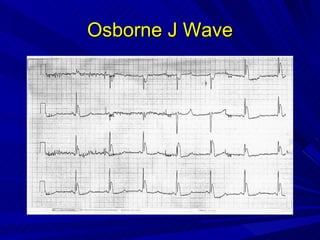
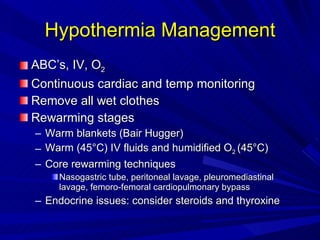
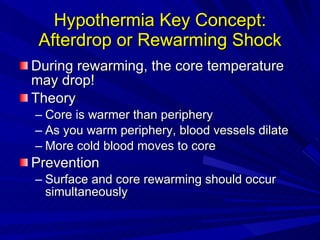
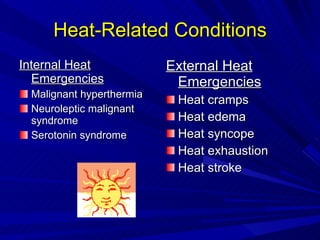
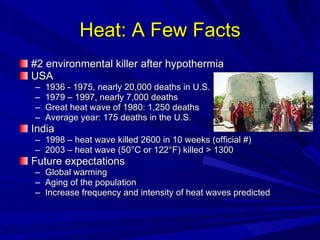
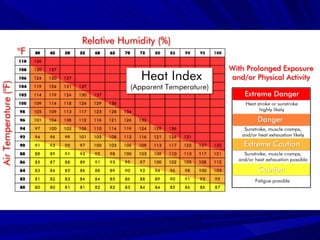
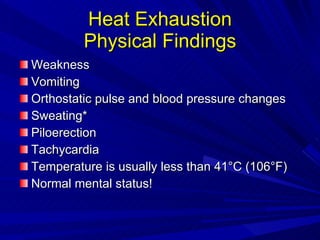
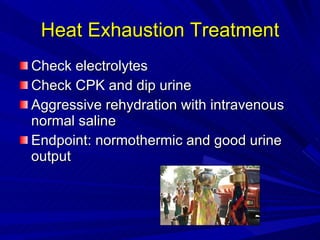
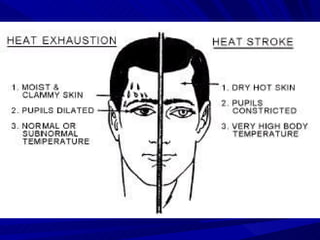
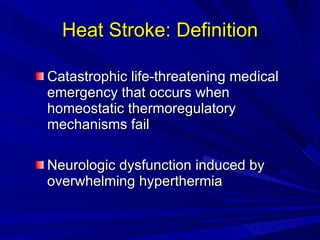
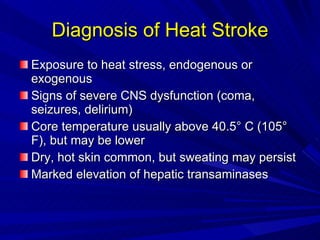
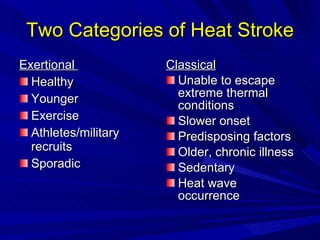
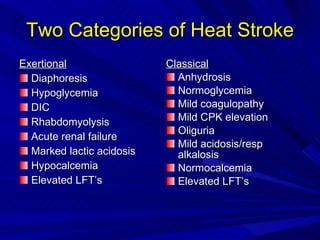
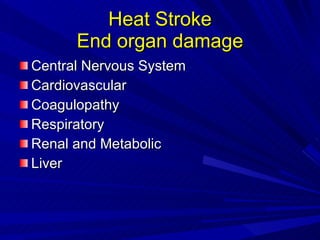
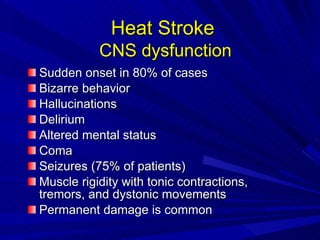
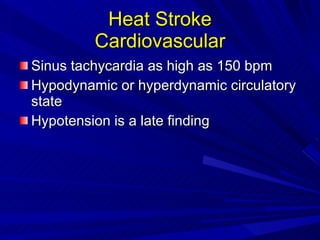
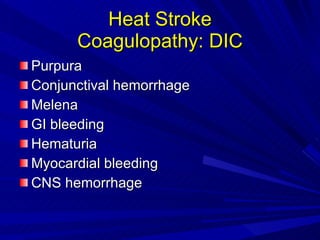
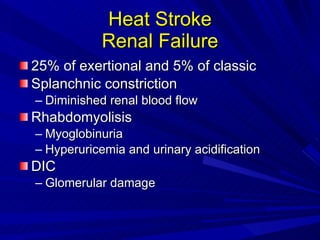
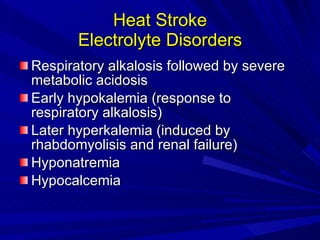
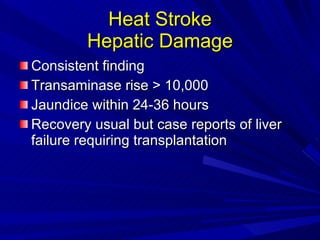
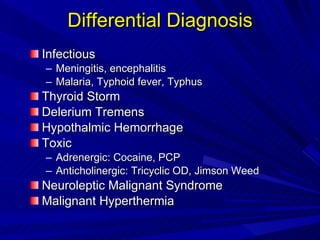
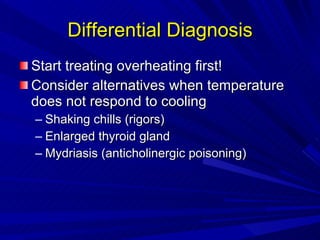
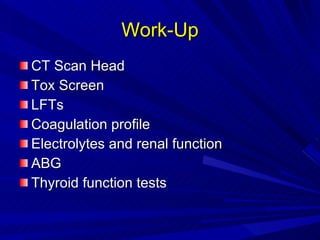
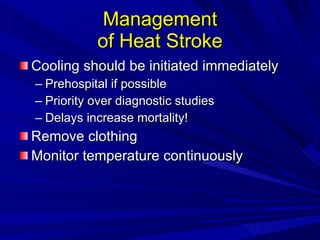
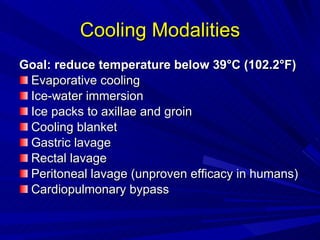
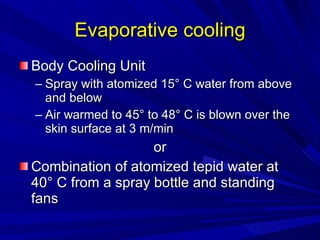
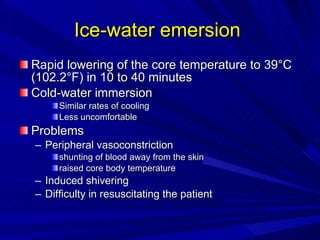
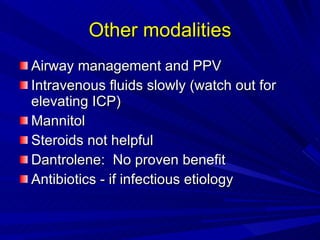
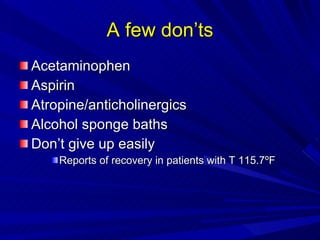
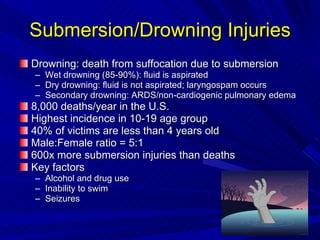
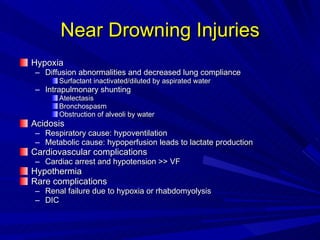
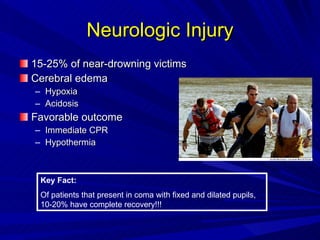
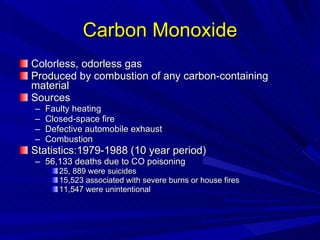
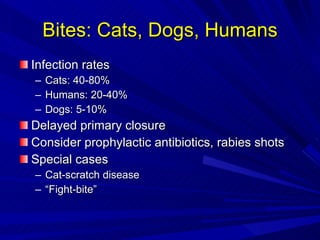
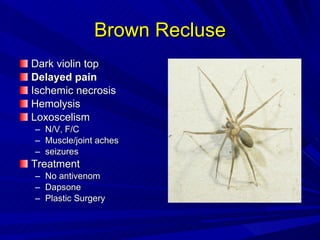
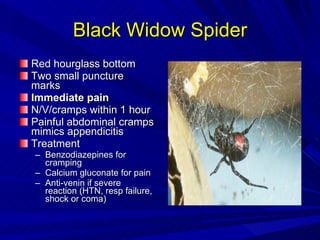
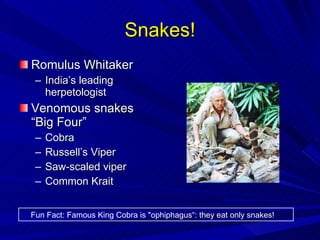
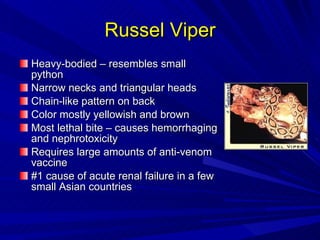
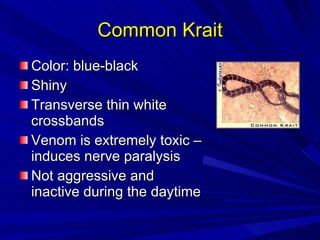
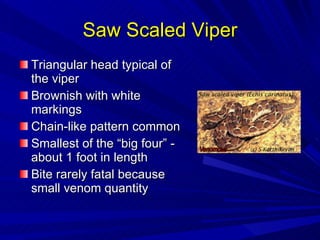
The document details various environmental injuries, including cold-related, heat-related, electrical injuries, and drowning, along with their clinical signs, management, and prevention strategies. It covers specific conditions such as frostbite, hypothermia, heat stroke, and interventions for electrical and drowning incidents, emphasizing urgent care and monitoring. Furthermore, it highlights the incidence of various injuries in different demographics and outlines approaches to treat bites and stings from animals.