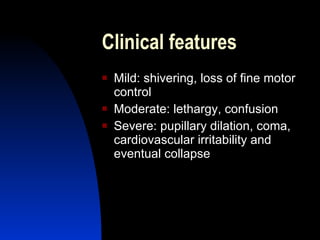
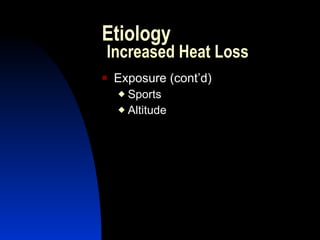
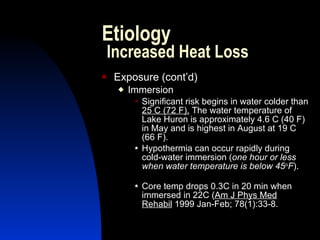
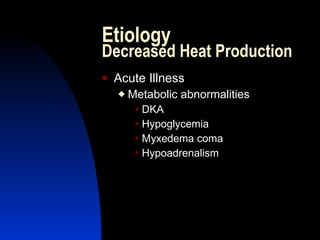
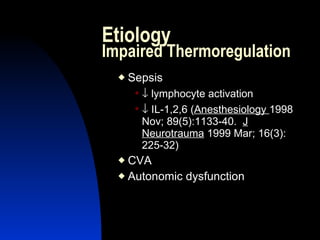
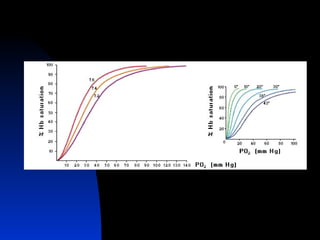
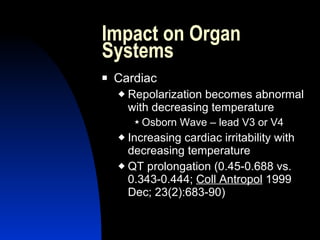
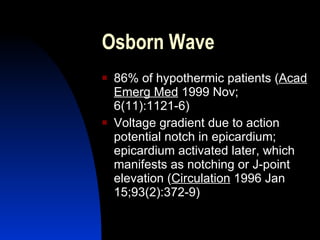
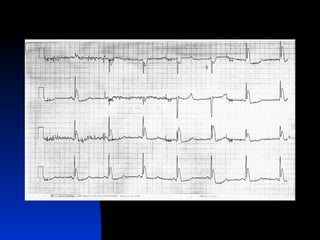
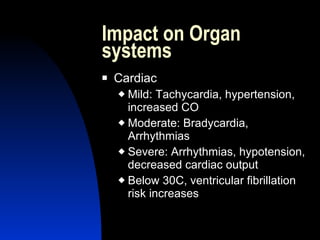
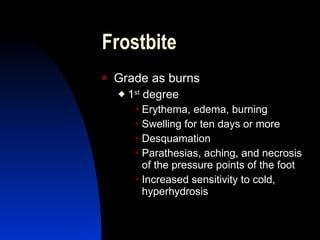
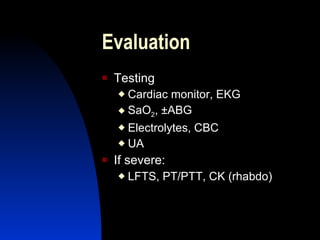
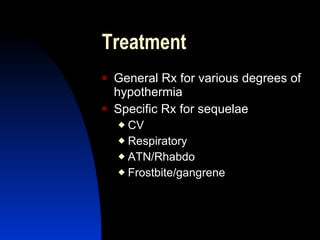
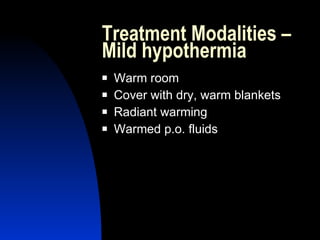
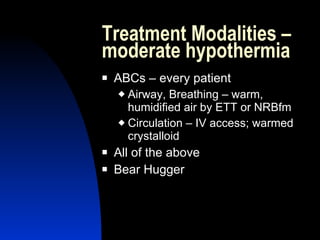
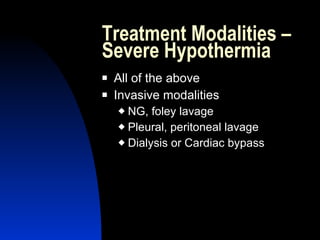
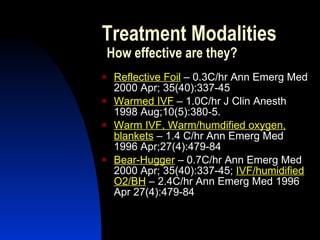
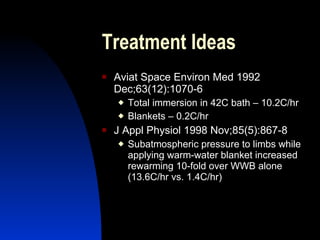
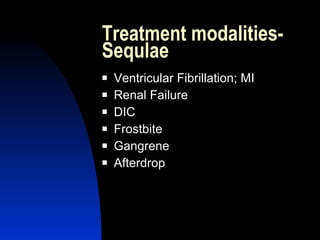
This document discusses hypothermia, including its definition, causes, effects on organ systems, identification, and treatment approaches. Key points include: 1) Hypothermia is defined as a core body temperature below 96.8°F and can be mild, moderate, or severe; 2) It is caused by increased heat loss or decreased heat production and impacts organ systems like the heart, brain, and kidneys; 3) Identification requires measuring low rectal temperature with a specialized thermometer and gentle patient handling; 4) Treatment aims to rewarm the body slowly through passive warming and may involve invasive approaches for severe hypothermia to avoid complications like afterdrop.