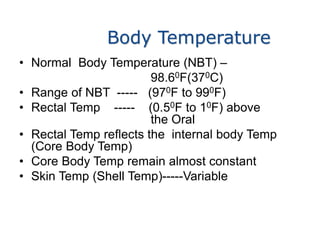
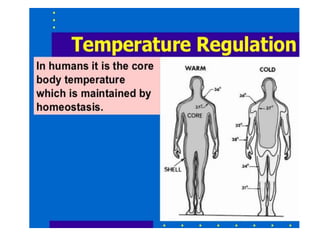
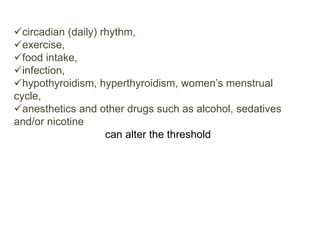
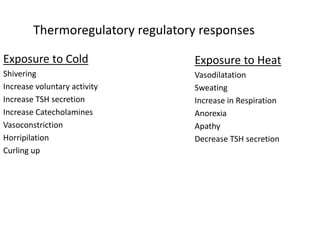
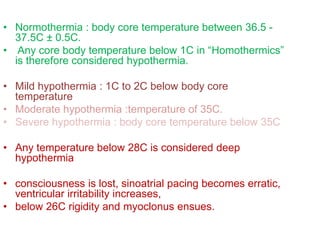
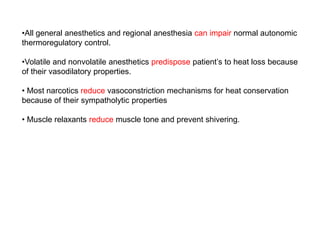
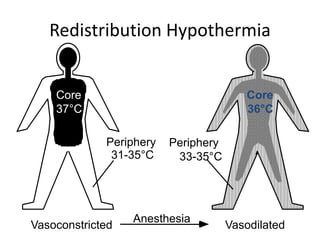
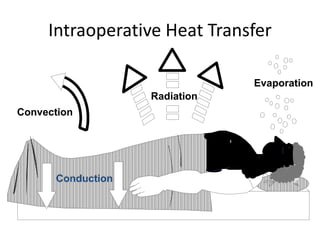
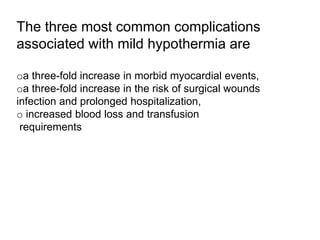
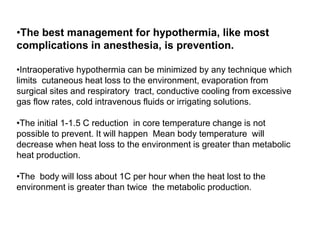
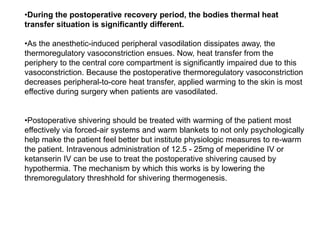
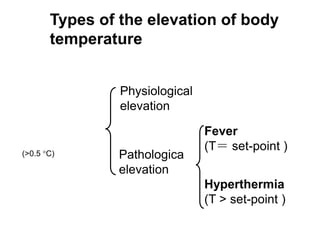
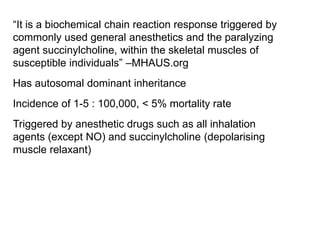
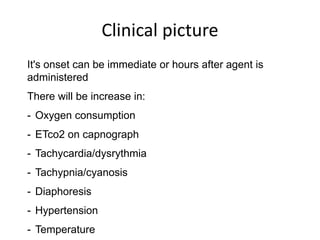
The document discusses temperature management in surgical patients. It covers normal body temperature, factors that can alter temperature, thermoregulatory responses to heat and cold, and classifications of hypothermia and hyperthermia. It also summarizes complications of hypothermia, prevention and treatment of intraoperative hypothermia, malignant hyperthermia, and management of hyperthermia and fever.


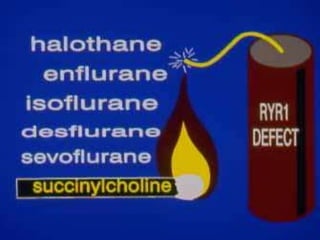
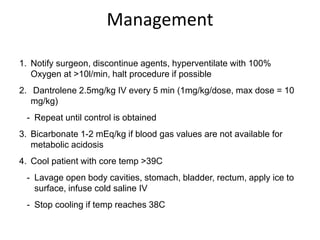
![Remember
"Some Hot Dude Better Give Iced Fluids Fast!"
(Hot dude = hypothermia):
Stop triggering agents
Hyperventilate/ Hundred percent oxygen
Dantrolene (2.5mg/kg)
Bicarbonate
Glucose and insulin
IV Fluids and cooling blanket
Fluid output monitoring/ Furosemide/ Fast
heart [tachycardia]](https://image.slidesharecdn.com/temperaturematters-160817172324/85/Temperature-matters-33-320.jpg)