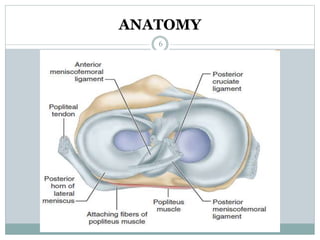
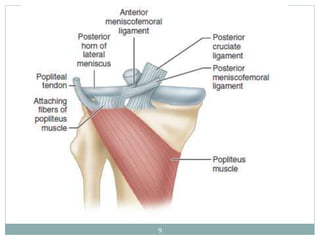
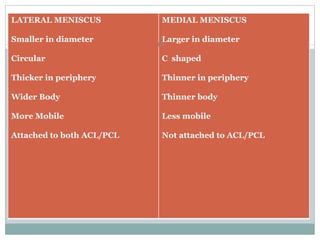
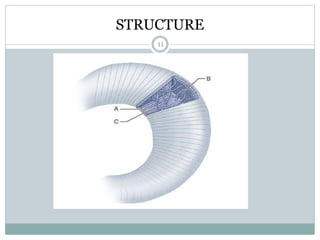
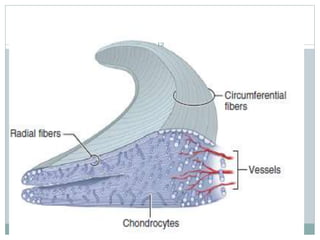
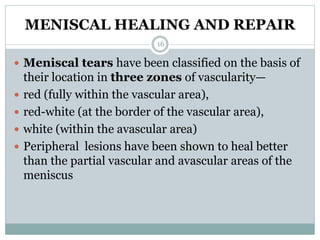
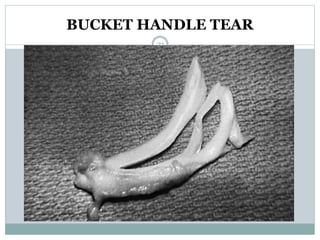
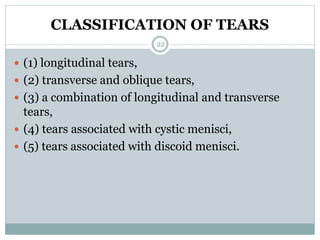
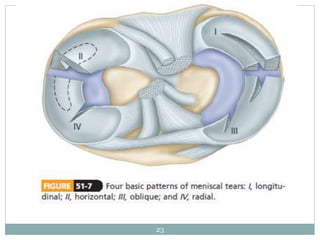
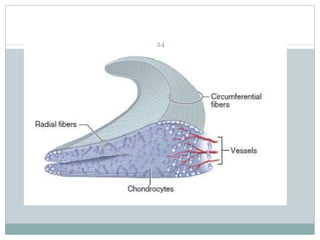
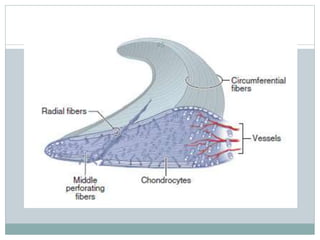
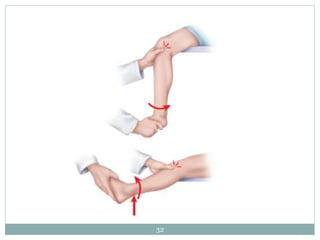
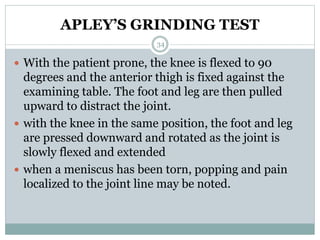
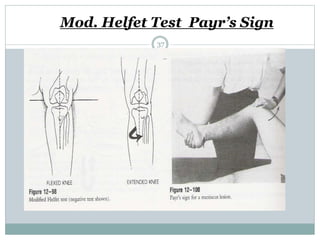
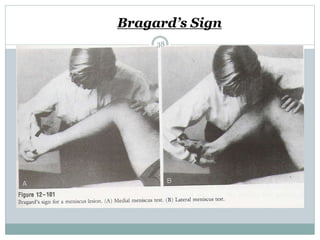
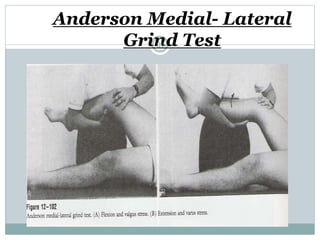
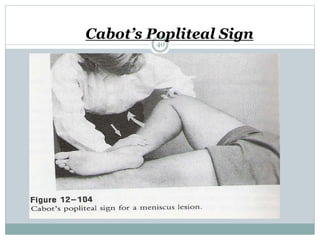
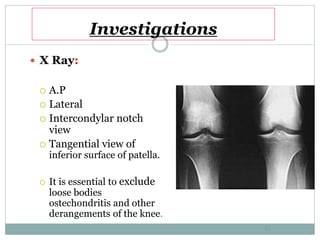
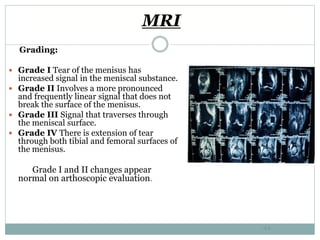
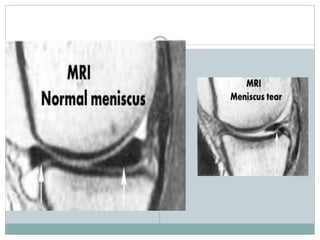
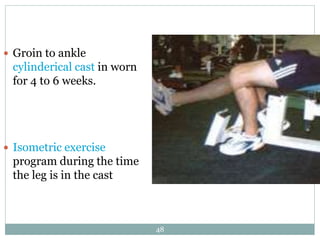
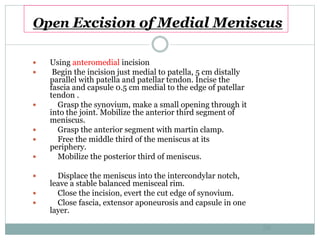
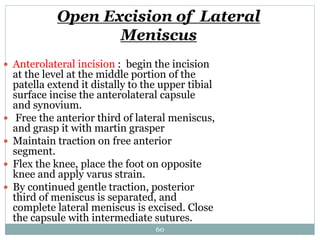
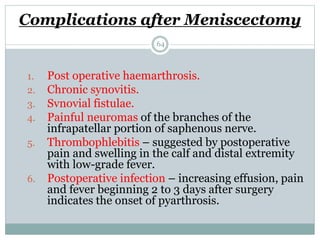
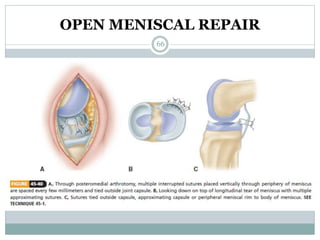
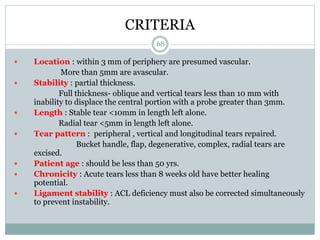
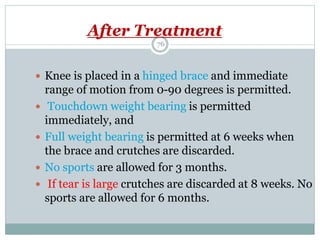
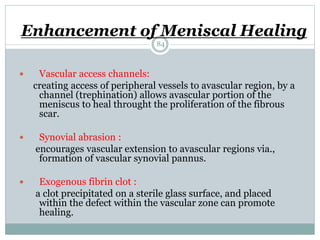
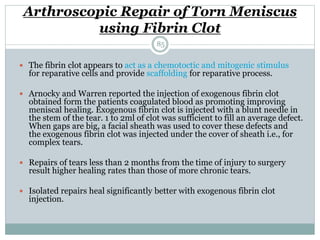
The document discusses meniscal injuries and pathology. It provides information on the anatomy and function of the menisci, as well as types of meniscal tears. The diagnosis of meniscal tears involves taking a history of the injury and examining for symptoms like joint line tenderness, effusion, and a locking sensation. Investigations may include x-rays, MRI, arthrography and arthroscopy. Treatment options discussed include non-surgical management for minor tears and surgical repair or resection for larger tears.