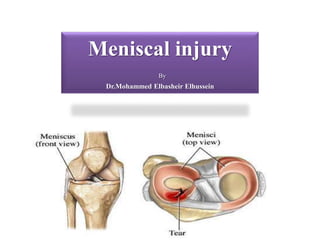
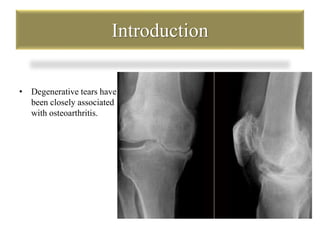
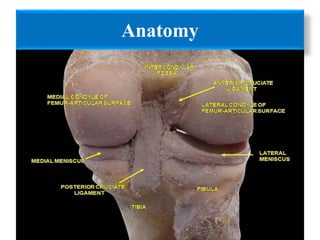
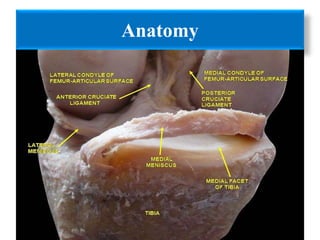
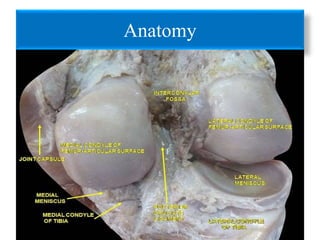
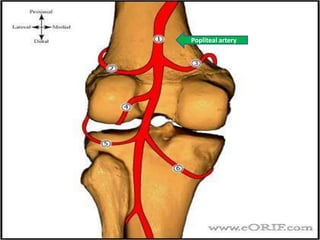
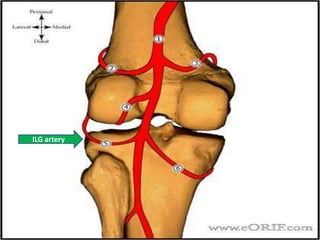
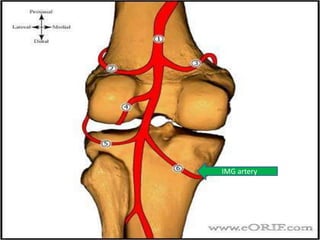
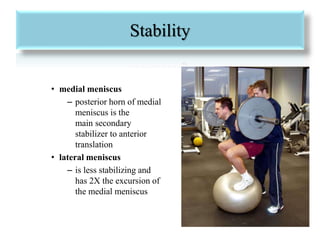
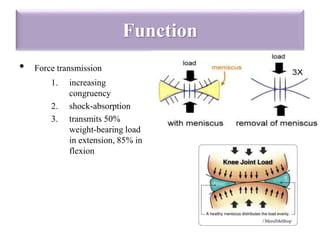
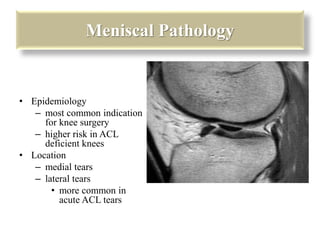
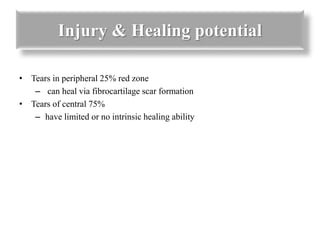
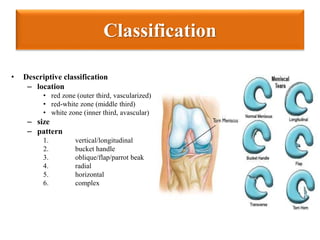
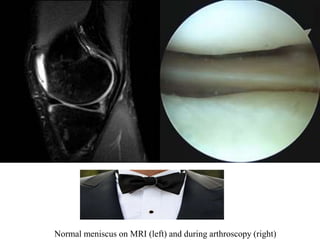
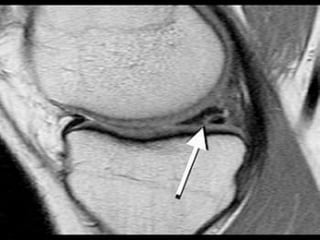
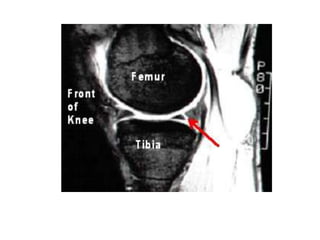
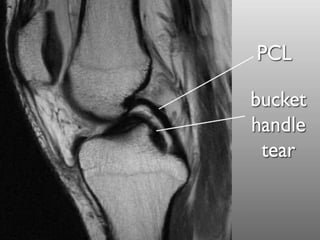
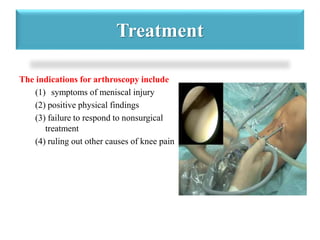
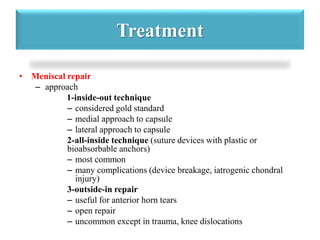
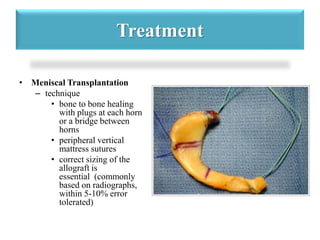
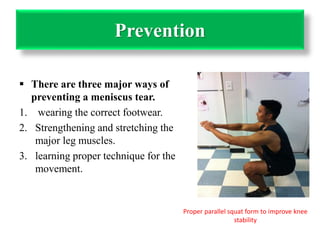
The document discusses meniscal injuries of the knee. It describes the anatomy and function of the menisci, types of meniscal tears, symptoms and diagnosis of tears. Treatment options include nonsurgical care, partial meniscectomy to remove torn parts, and meniscal repair surgery which is best for peripheral, vertical tears. While removal addresses pain, it increases risk for osteoarthritis long term. The goal of repair is to preserve as much viable meniscal tissue as possible for cartilage protection.