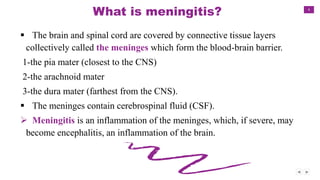
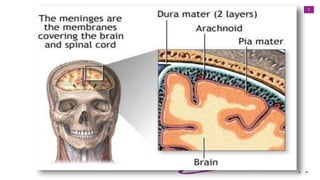
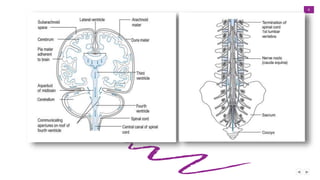
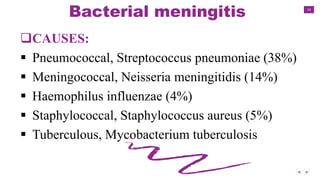
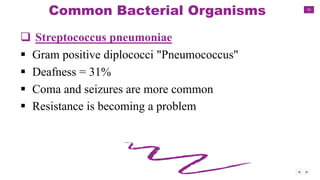
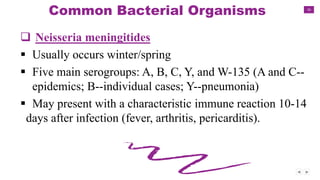
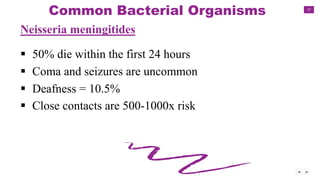
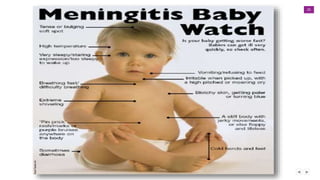
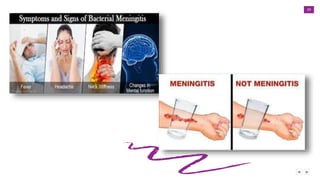
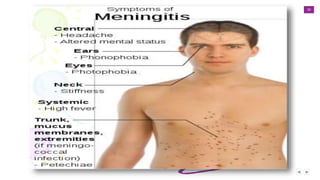
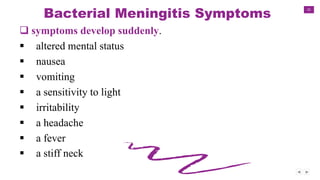
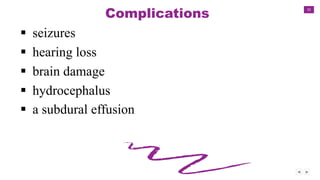
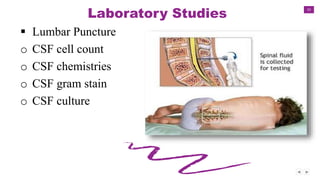
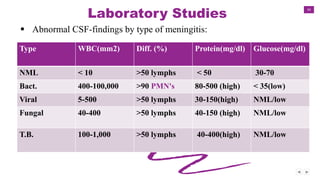
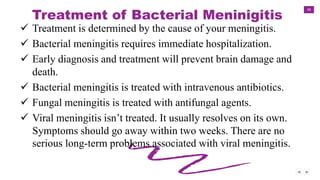
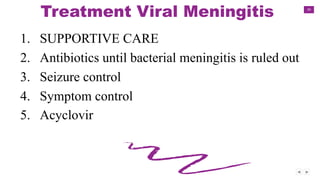
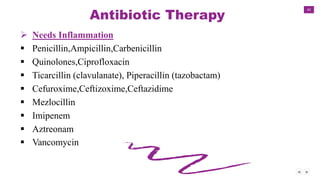
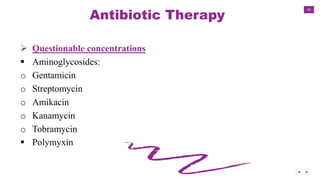
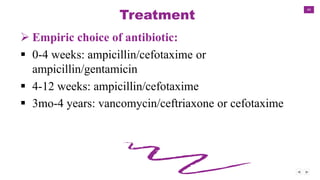
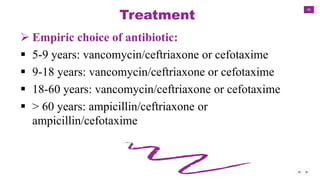
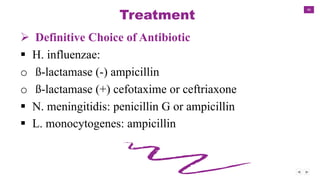
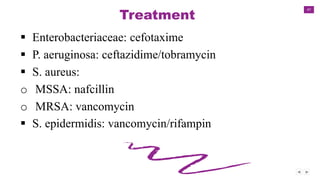
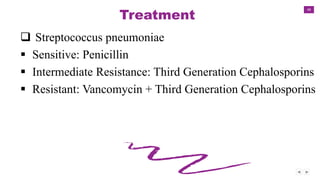
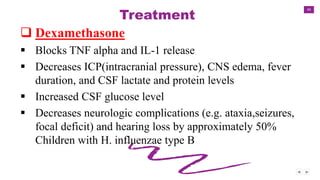
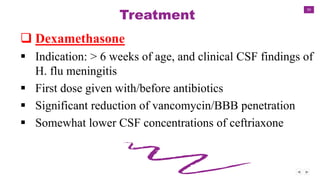
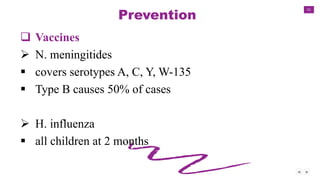
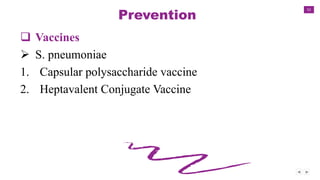
Meningitis is an inflammation of the meninges, which cover the brain and spinal cord. It can be caused by viruses, bacteria, or fungi. Bacterial meningitis requires urgent treatment with antibiotics to prevent death. Common symptoms include headache, fever, and neck stiffness. Diagnosis involves lumbar puncture and analyzing cerebrospinal fluid. Treatment depends on the cause but antibiotics are given for bacterial meningitis. Vaccines can prevent some types of bacterial meningitis.