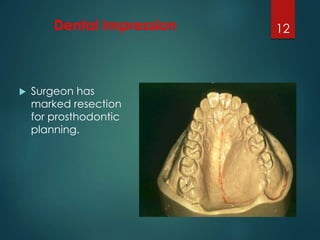
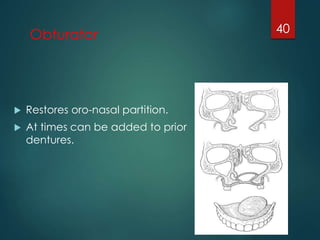
Maxillofacial prosthetics aims to restore function and aesthetics after trauma or surgery. There are several types of prosthetics used including immediate, transitional, and definitive obturators. Immediate obturators are inserted after surgery to aid healing and function, while definitive obturators are longer term replacements created once healing is complete. Congenital defects like cleft lip and palate are also rehabilitated, usually through early surgical closure along with prosthetic appliances for feeding, speech, and aesthetics.