This document discusses considerations for fixed prosthodontics in patients with compromised periodontal health. Key points include:
- Periodontal health plays an important role in the longevity of restorations, and defective prostheses can contribute to periodontal disease progression. Successful treatment requires cooperation between periodontists and prosthodontists.
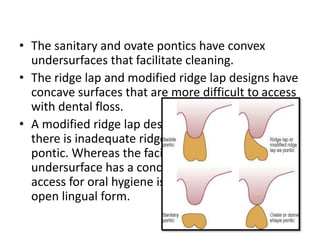
- Periodontal issues must be resolved before restorative treatment to avoid tensions on the periodontium from tooth movement. Supragingival margins and open embrasures are preferred for periodontal health.
- Temporary splinting can help determine the prognosis of a permanent restoration in periodontally compromised patients. Occlusion should not interfere with plaque control.