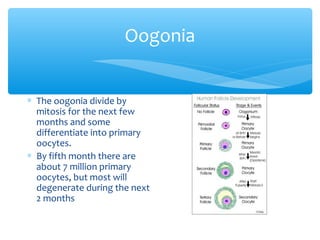
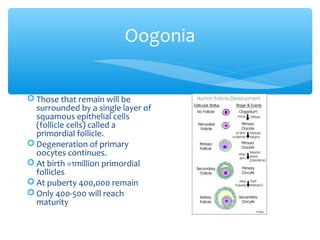
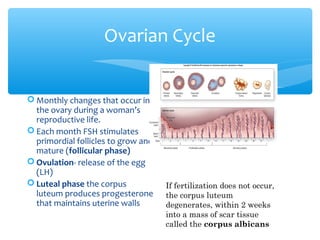
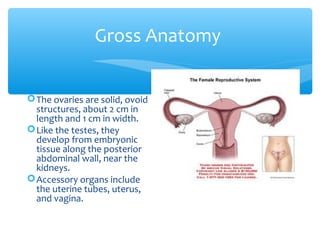
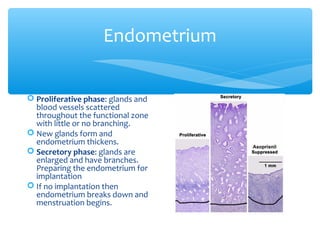
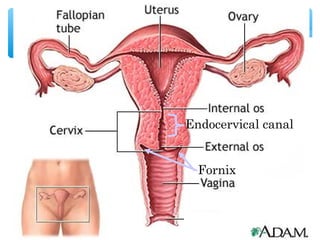
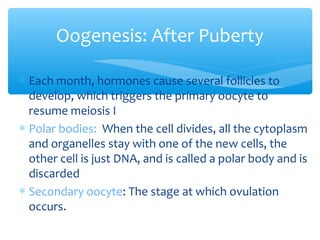
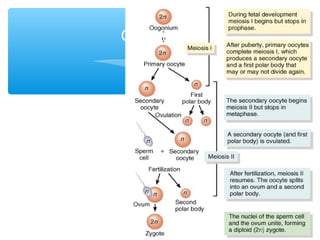
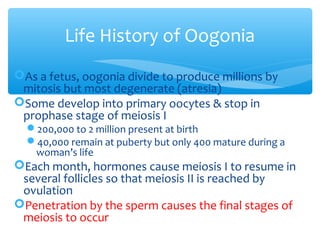
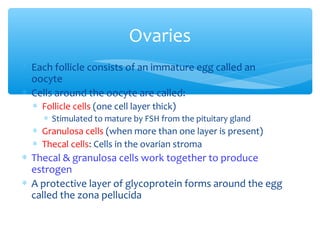
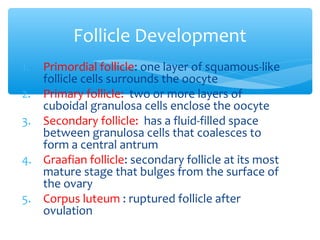
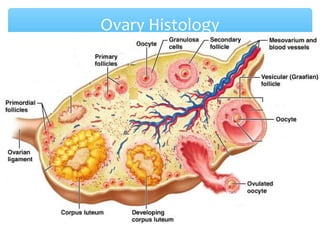
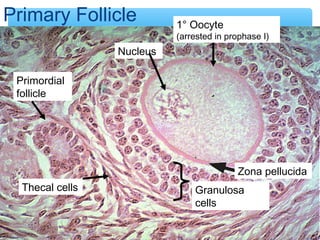
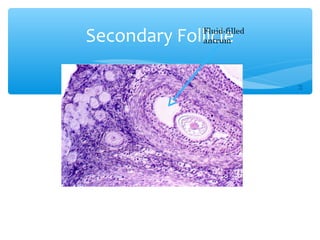
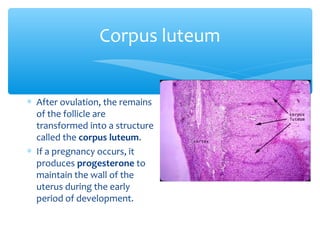
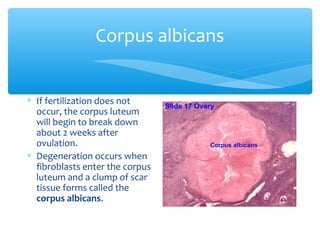
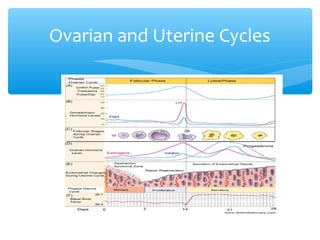
The female reproductive system produces a finite number of eggs during fetal development. During puberty, hormones cause follicles in the ovaries to mature and release eggs, with only a small number reaching maturity. If an egg is fertilized, it develops in the uterus, whose lining changes each month in preparation. If not fertilized, the corpus luteum degrades and menstruation occurs.