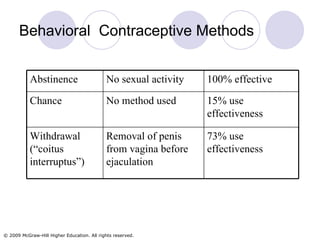
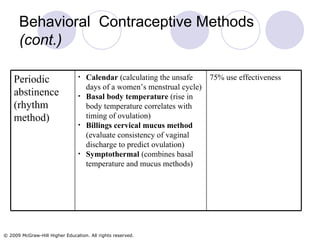
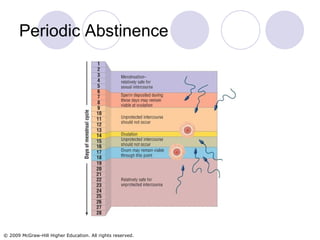
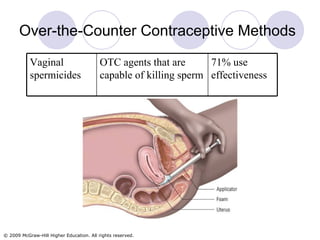
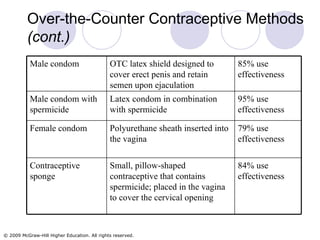
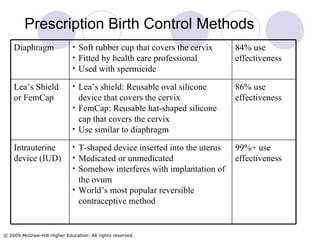
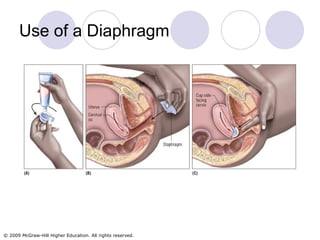
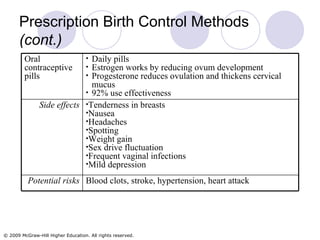
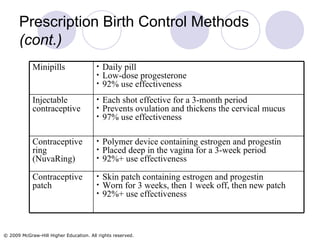
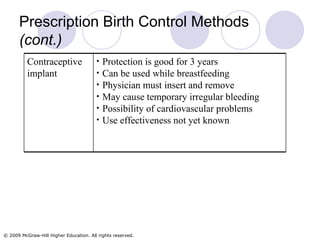
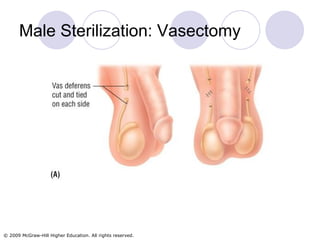
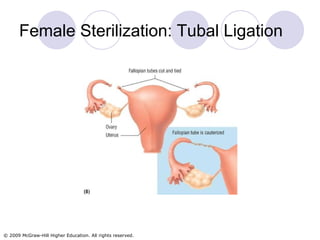
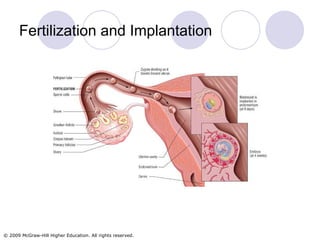
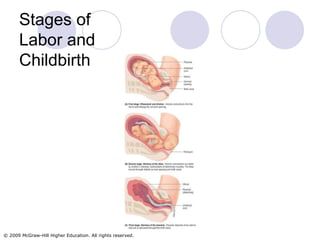
This chapter discusses various methods of fertility management, including contraception and fertility treatments. It covers behavioral, over-the-counter, and prescription contraceptive methods, as well as infertility treatments like fertility drugs, artificial insemination, and assisted reproductive technologies. The chapter also addresses pregnancy, childbirth processes like labor and delivery, and infertility issues and their potential solutions.