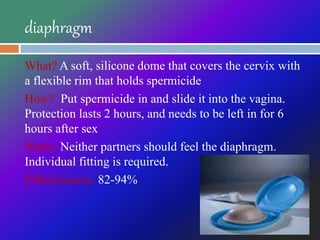
The document discusses various methods of contraception, including their effectiveness and how they work. It covers barrier methods like condoms and diaphragms, hormonal methods like pills and implants, intrauterine devices (IUDs), fertility awareness methods, emergency contraception, and permanent sterilization methods. Factors to consider when choosing a method include cost, effectiveness against pregnancy and STDs, safety, comfort, and reversibility. Effectiveness ranges from highly effective long-acting reversible methods like IUDs to less effective options like withdrawal.