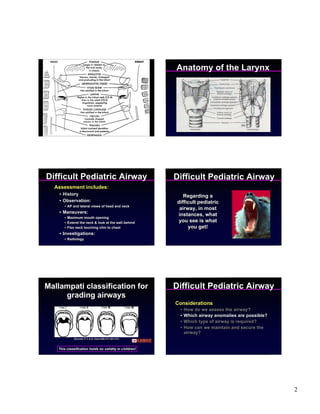
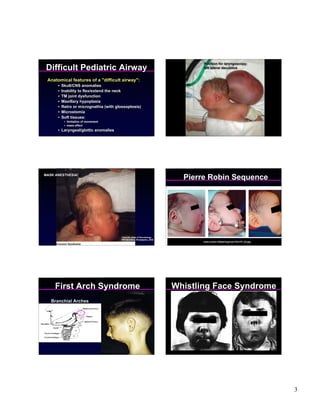
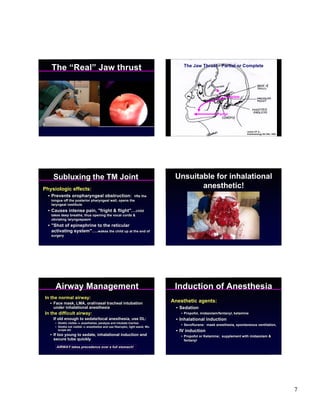
1) The document discusses managing difficult pediatric airways, noting assessments that should be done and potential airway anomalies.
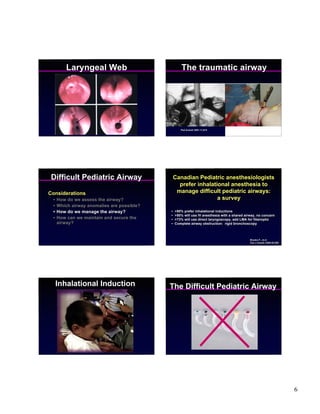
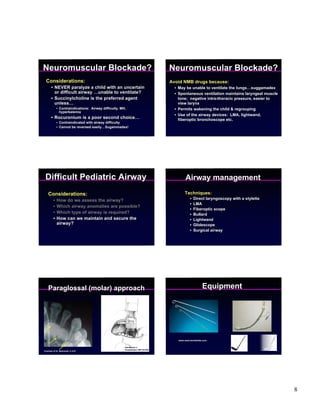
2) It describes various techniques that can be used to secure the airway depending on the child's condition, including inhalational induction, fiberoptic intubation, LMAs, and surgical airways if needed.
3) It emphasizes the importance of avoiding neuromuscular blockade in children with uncertain or difficult airways so spontaneous ventilation and regrouping are possible if needed. Maintaining the airway takes priority over other considerations like a full stomach.