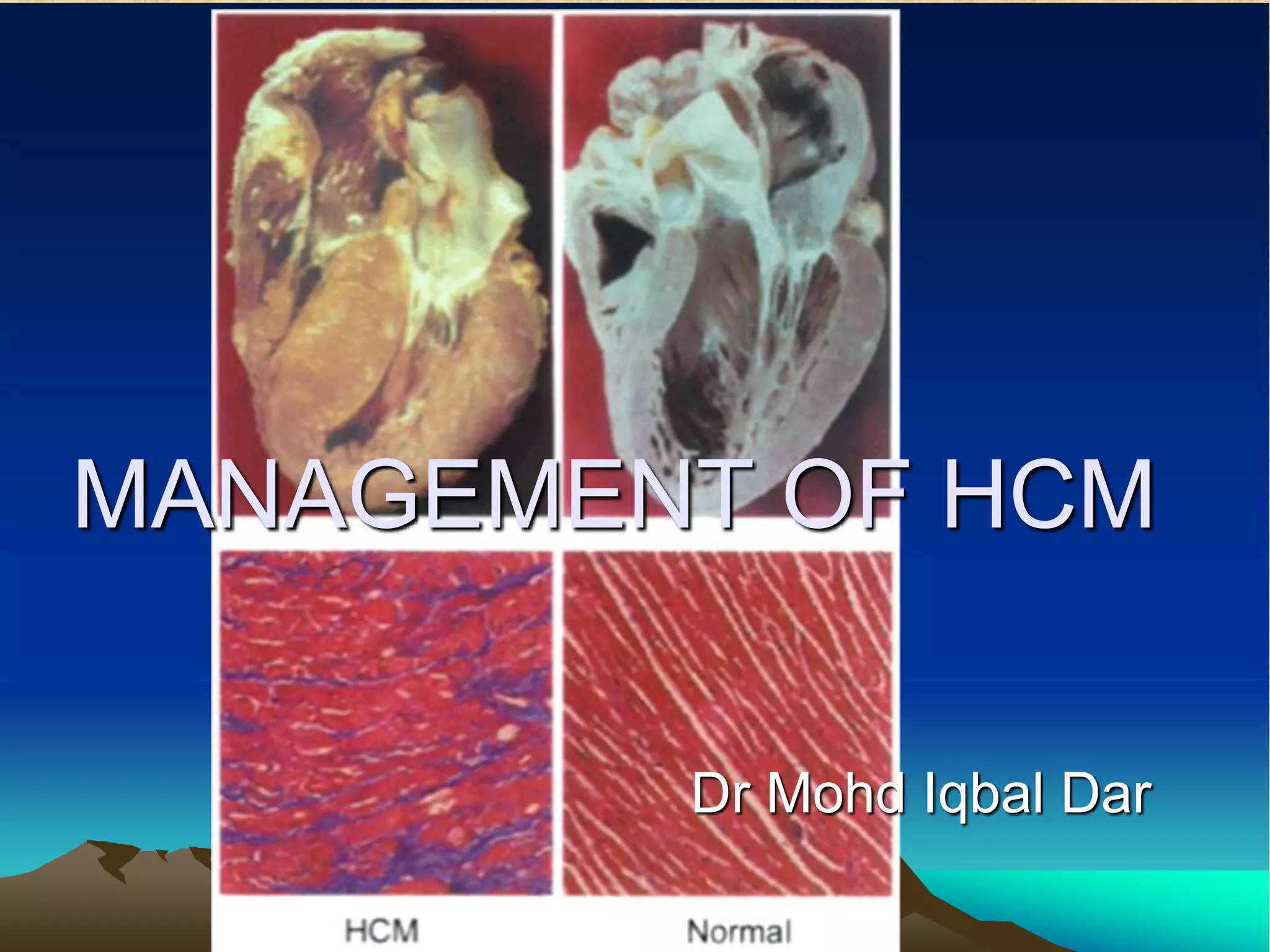
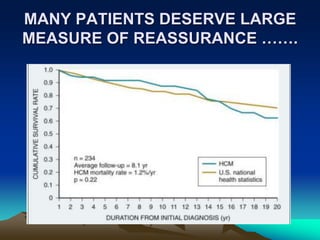
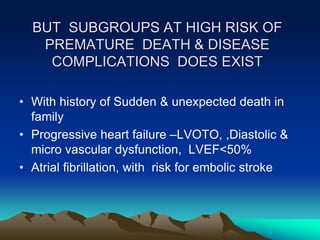
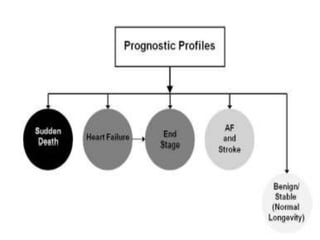
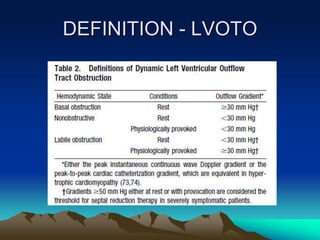
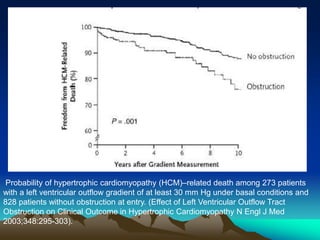
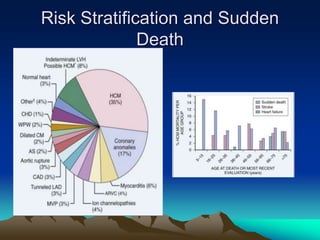
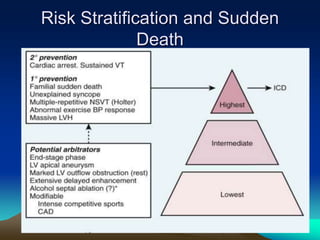
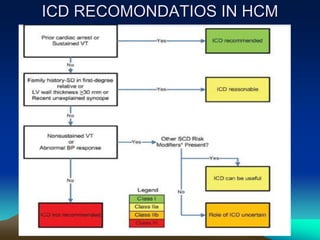
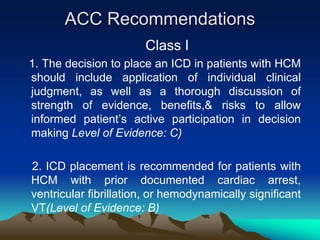
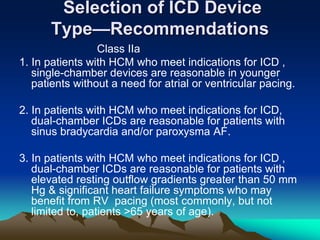
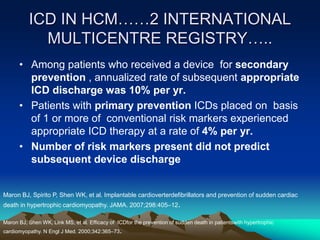
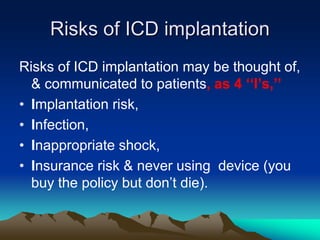
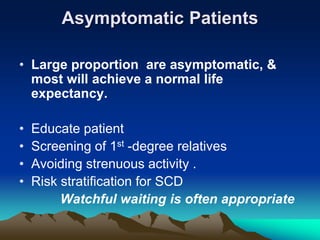
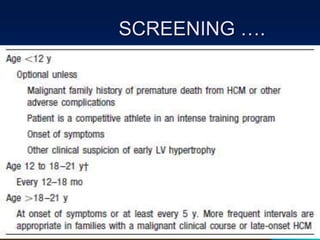
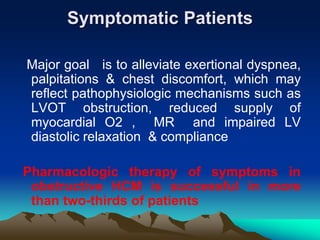
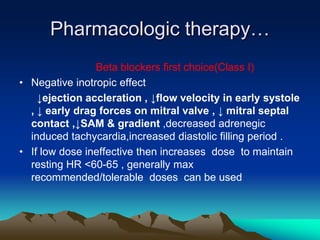
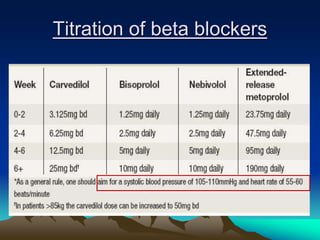
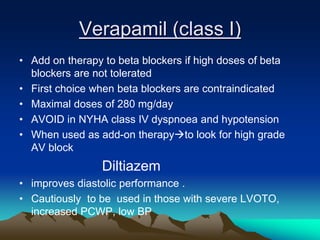
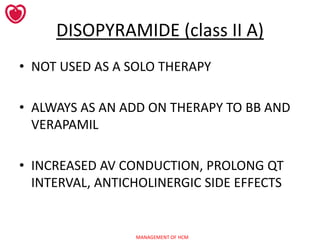
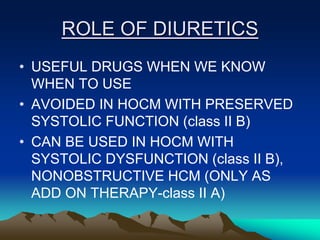
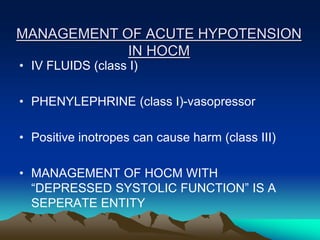
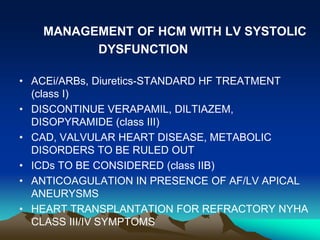
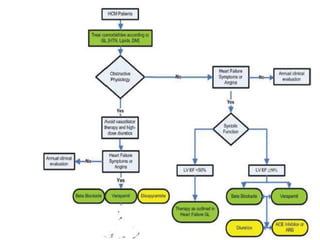
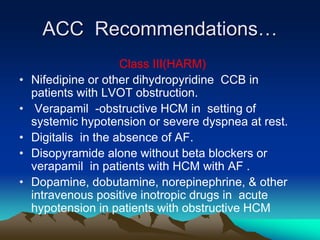
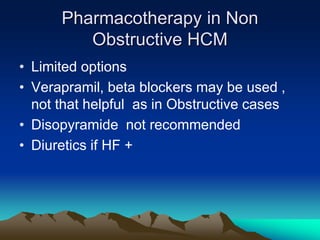
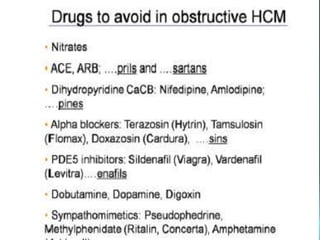
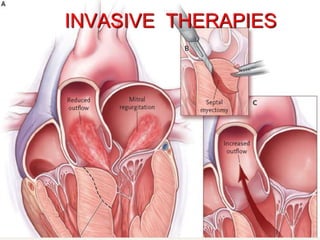
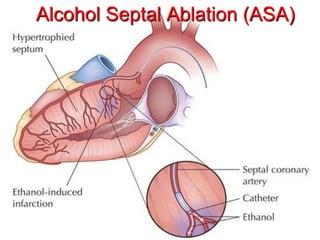
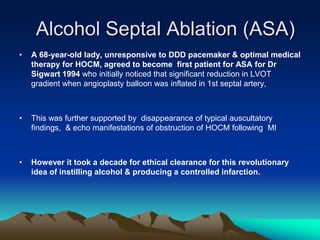
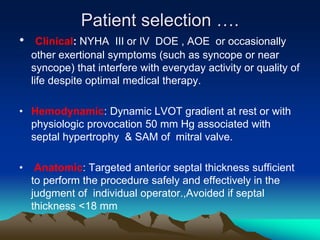
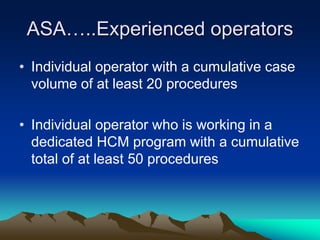
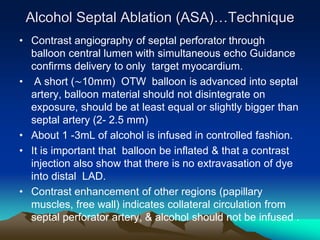
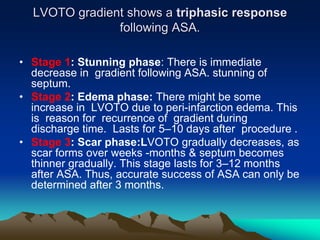
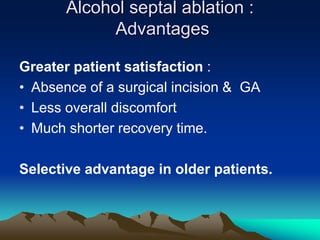
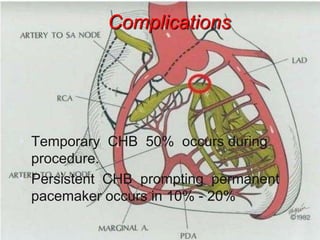
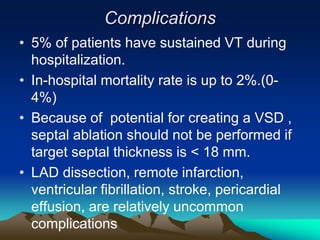
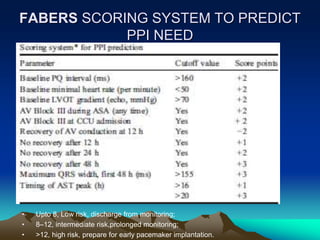
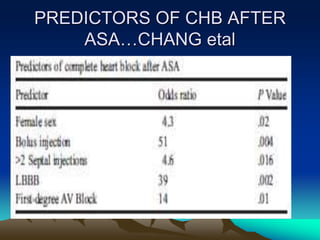
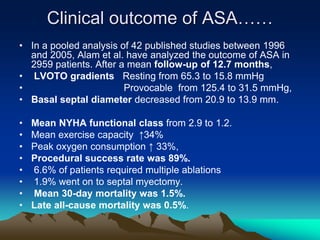
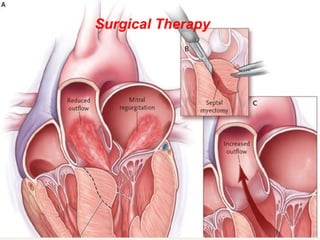
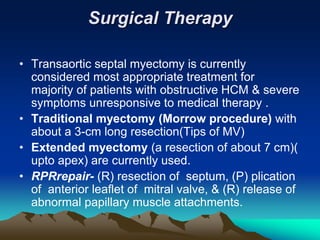
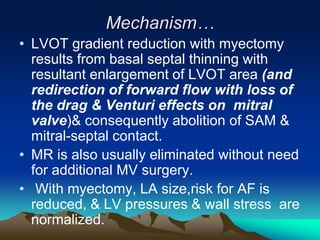
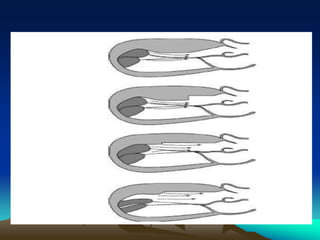
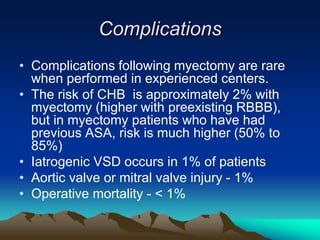
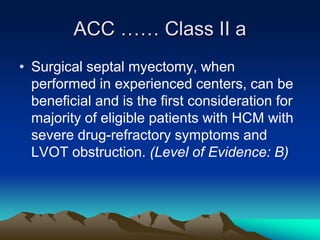
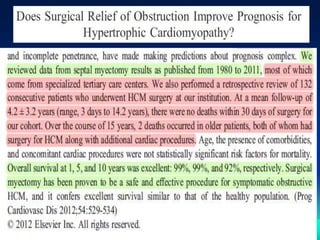
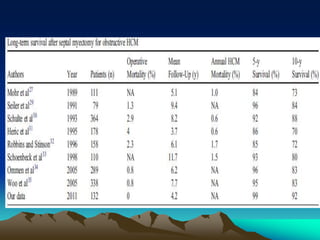
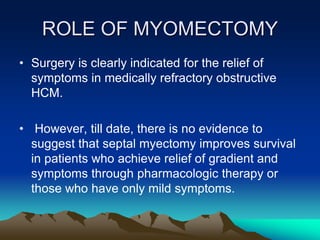
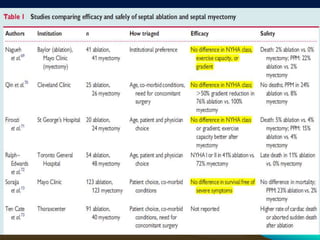
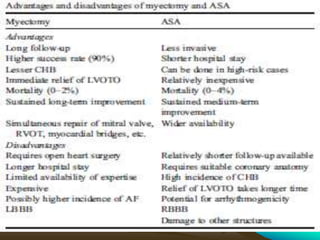
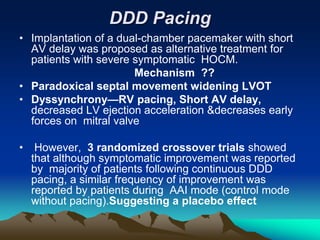
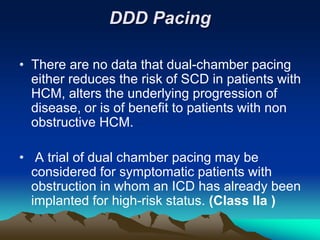
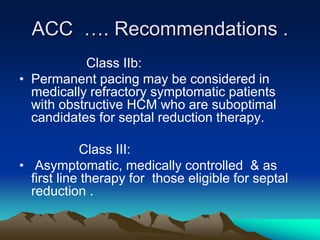
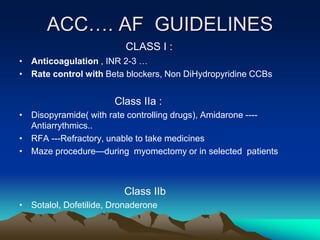
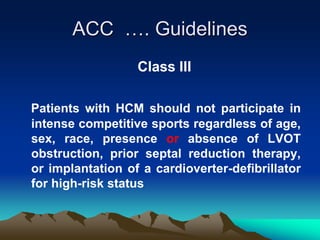
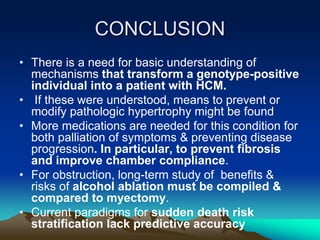
This document discusses the management of hypertrophic cardiomyopathy (HCM). It covers the natural history of HCM, risk stratification including the role of implantable cardioverter defibrillators, pharmacological treatments, and invasive treatments such as alcohol septal ablation and surgical myectomy. Key points discussed include the use of beta blockers as first-line pharmacological therapy, guidelines for ICD implantation, the technique and outcomes of alcohol septal ablation versus surgical myectomy, and recommendations for experienced centers to perform these invasive procedures.