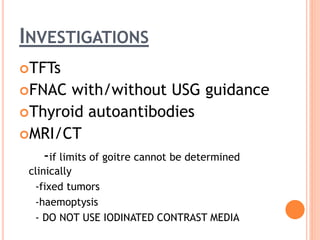
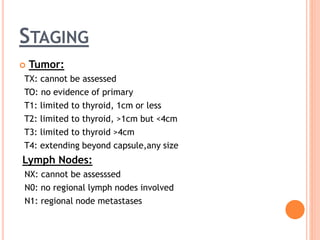
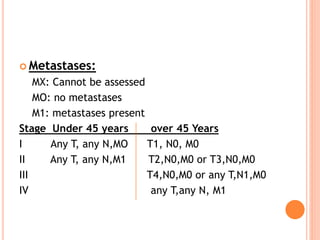
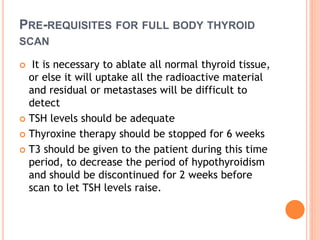
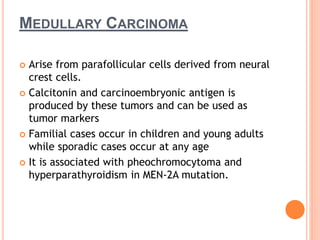
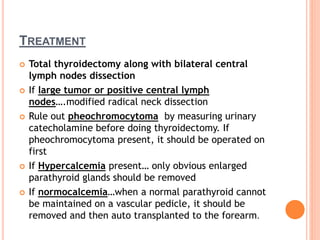
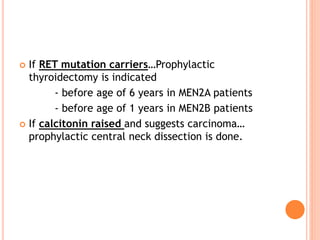
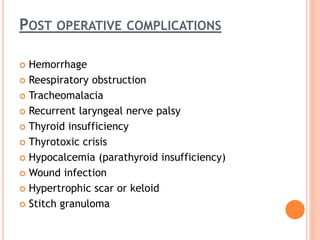
This document discusses malignant thyroid tumors. It begins by classifying the main types: papillary carcinoma (60%), follicular carcinoma (20%), anaplastic carcinoma (10%), and medullary carcinoma (5%). Risk factors and presentations are described. Investigations include thyroid function tests, FNAC biopsy, and imaging. Staging depends on tumor size, lymph node involvement, and presence of metastases. Well-differentiated tumors like papillary and follicular carcinoma can be treated with surgery and radioactive iodine. Medullary carcinoma is associated with genetic mutations. Anaplastic carcinoma has a poor prognosis despite aggressive treatment. Post-operative complications are also reviewed.