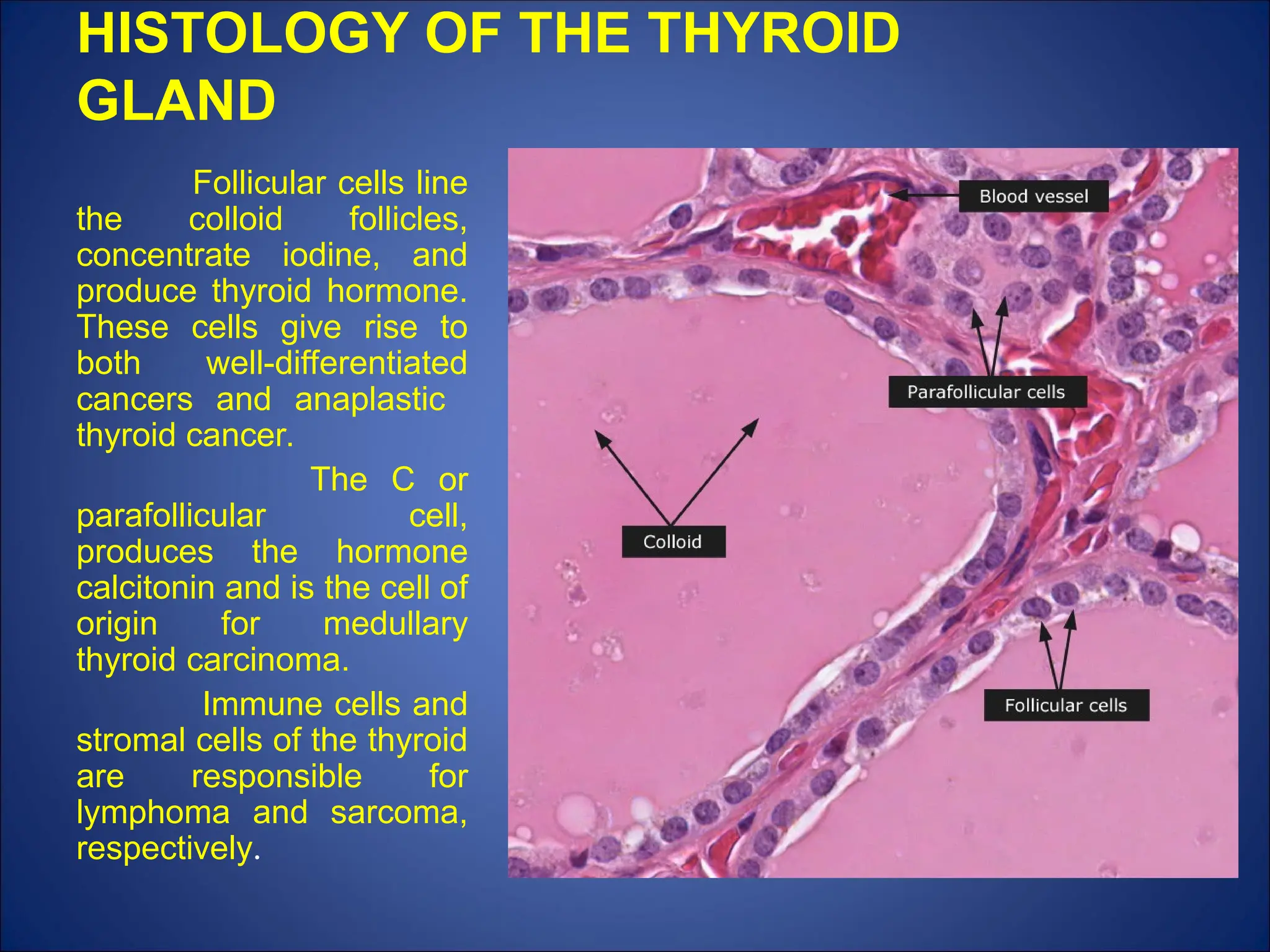
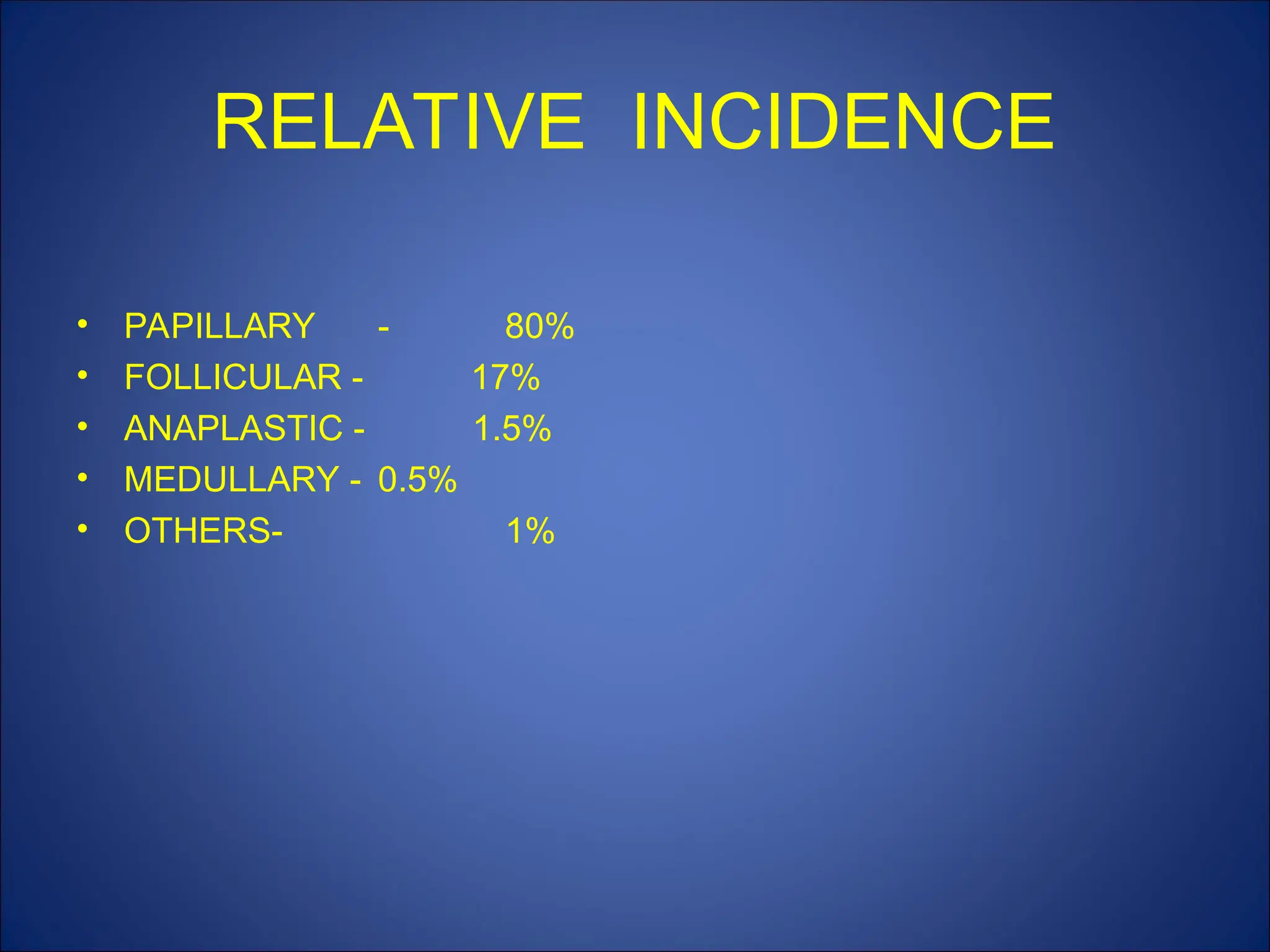
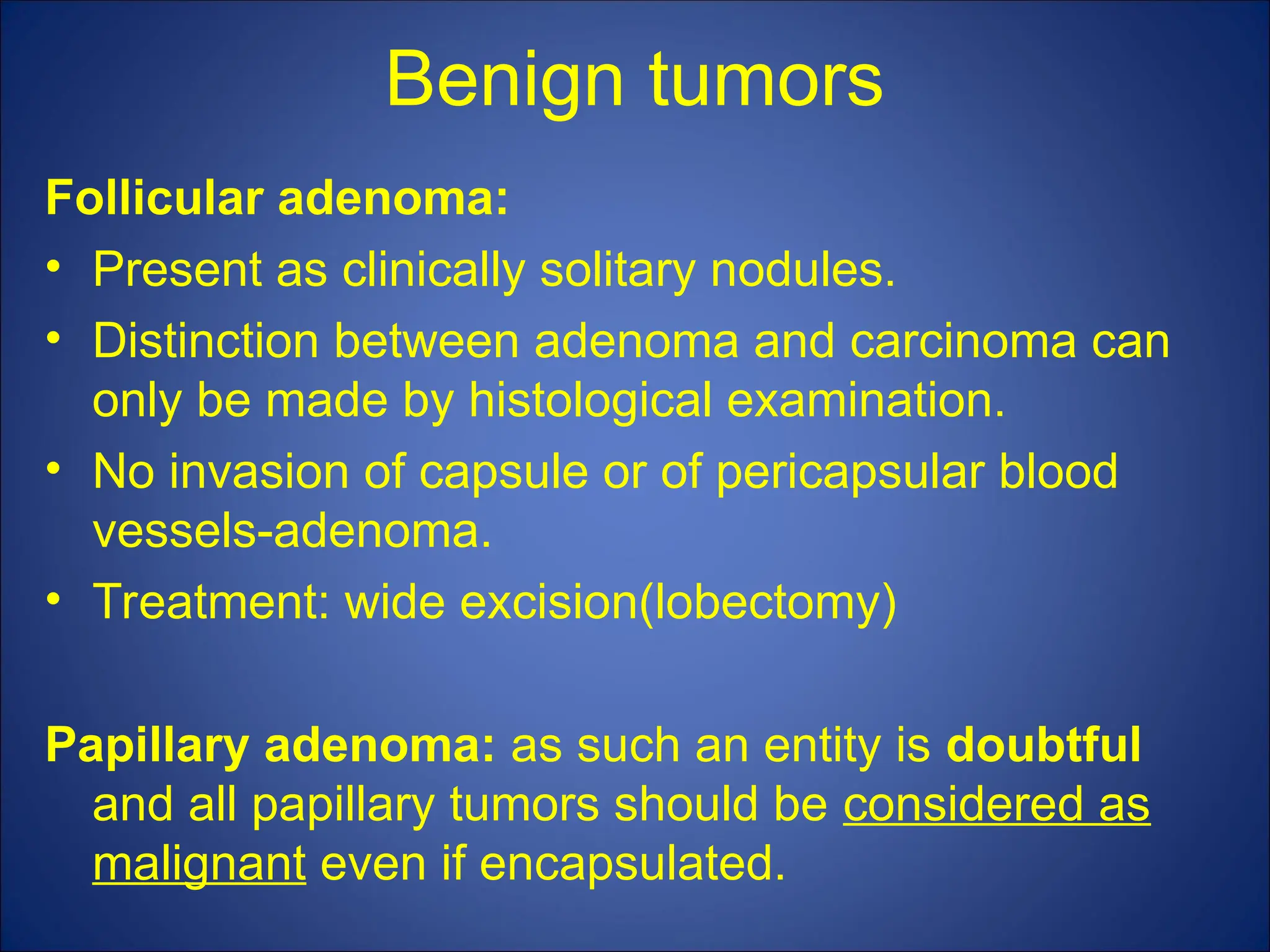
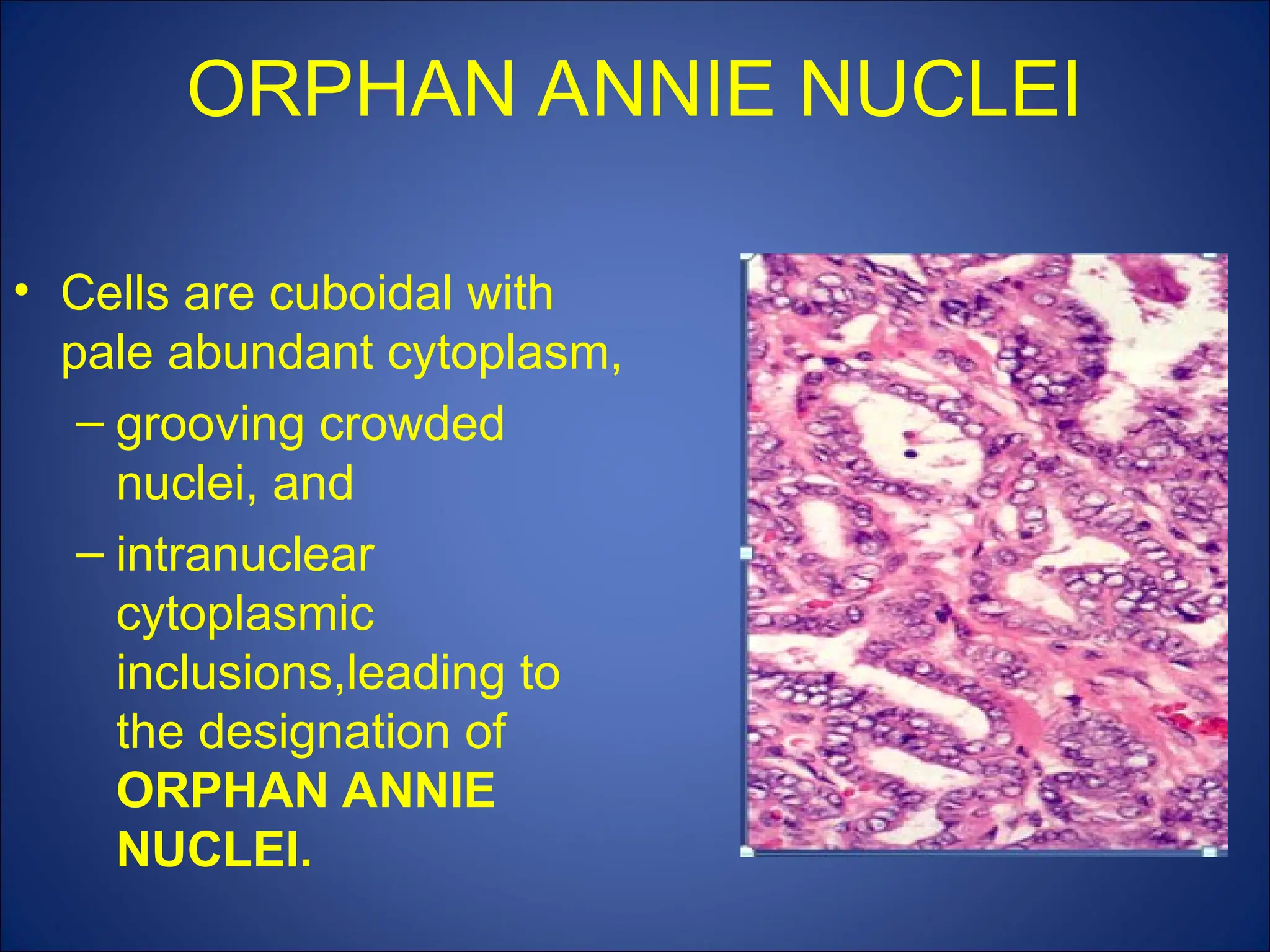
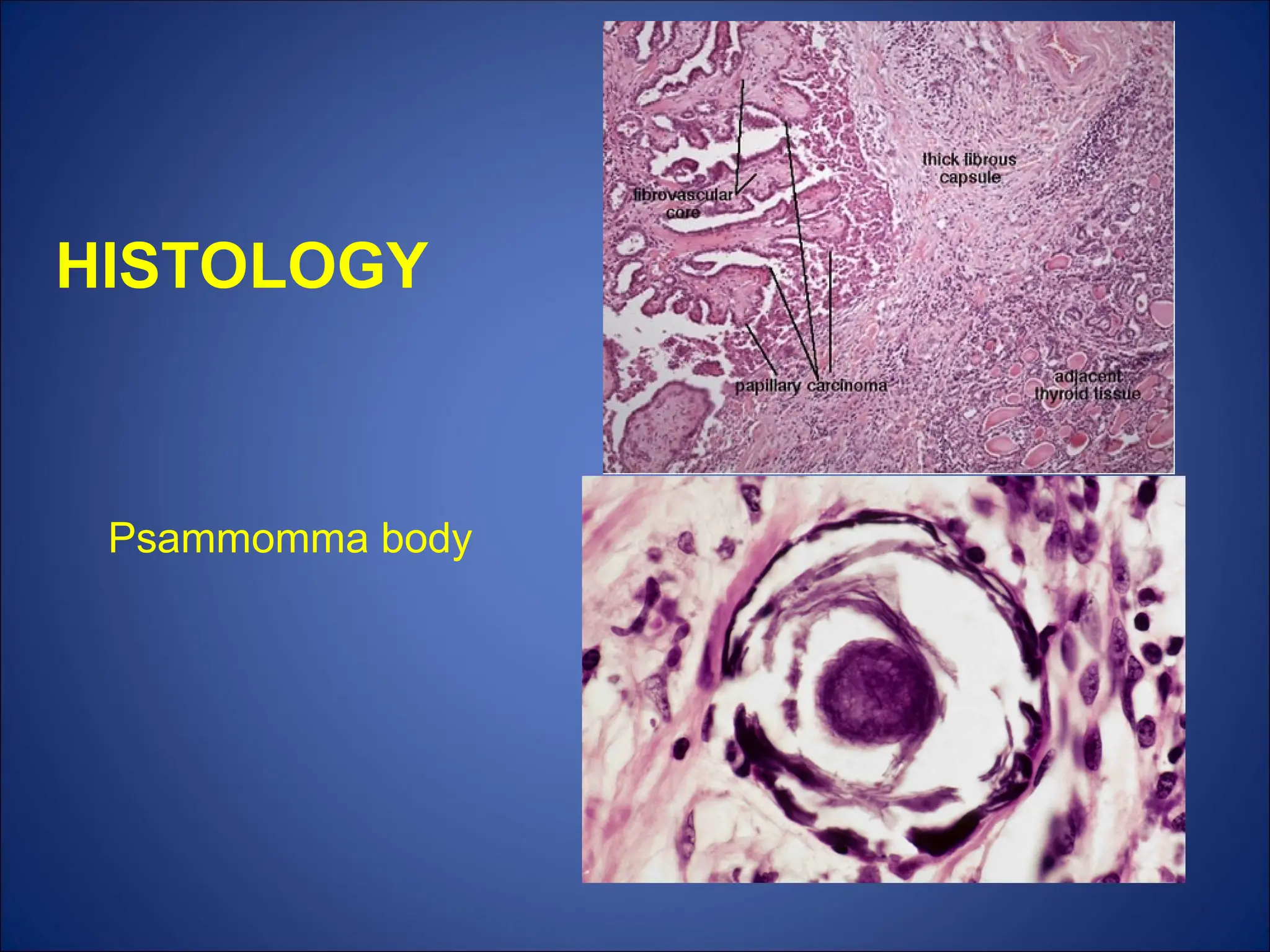
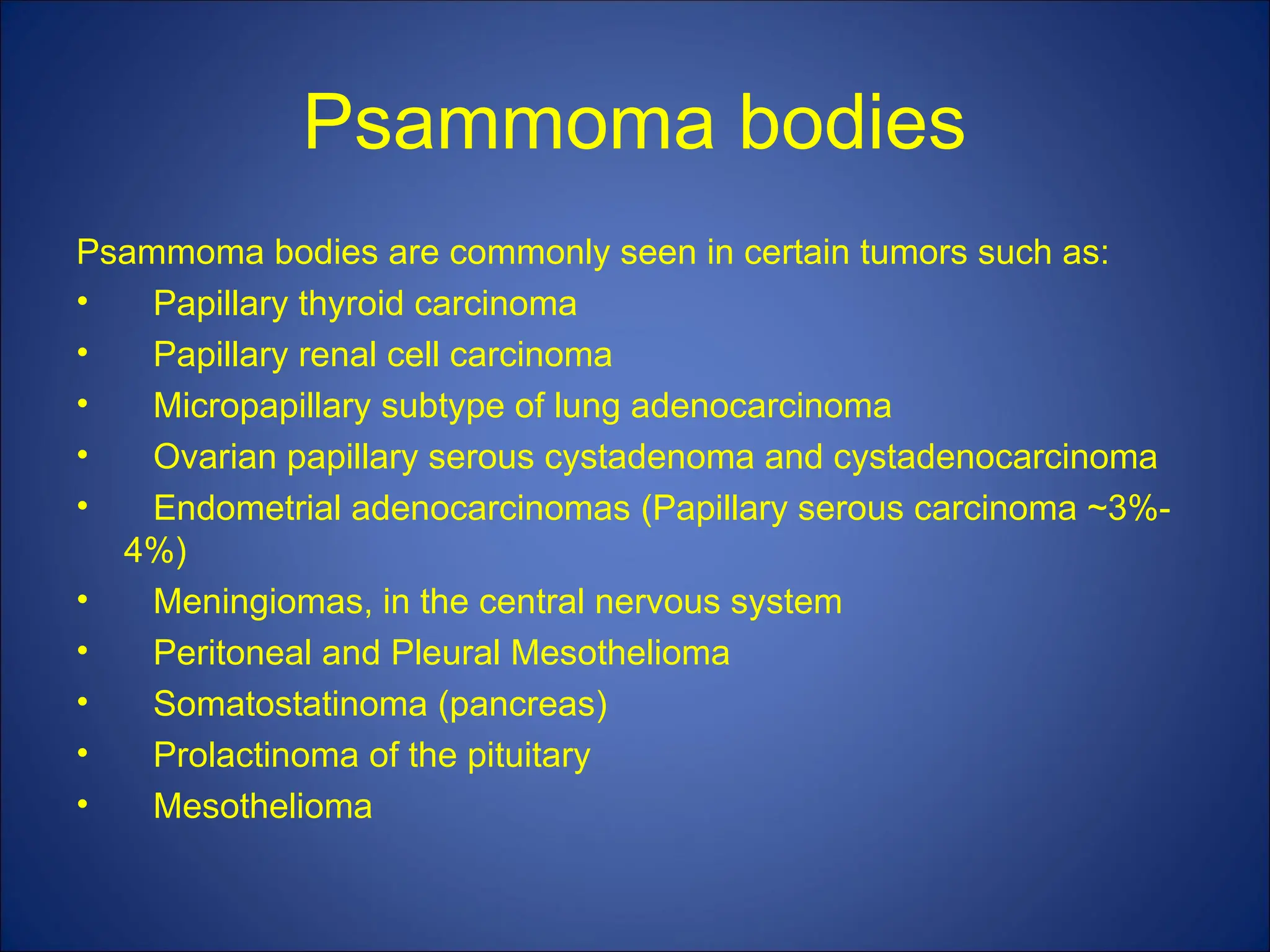
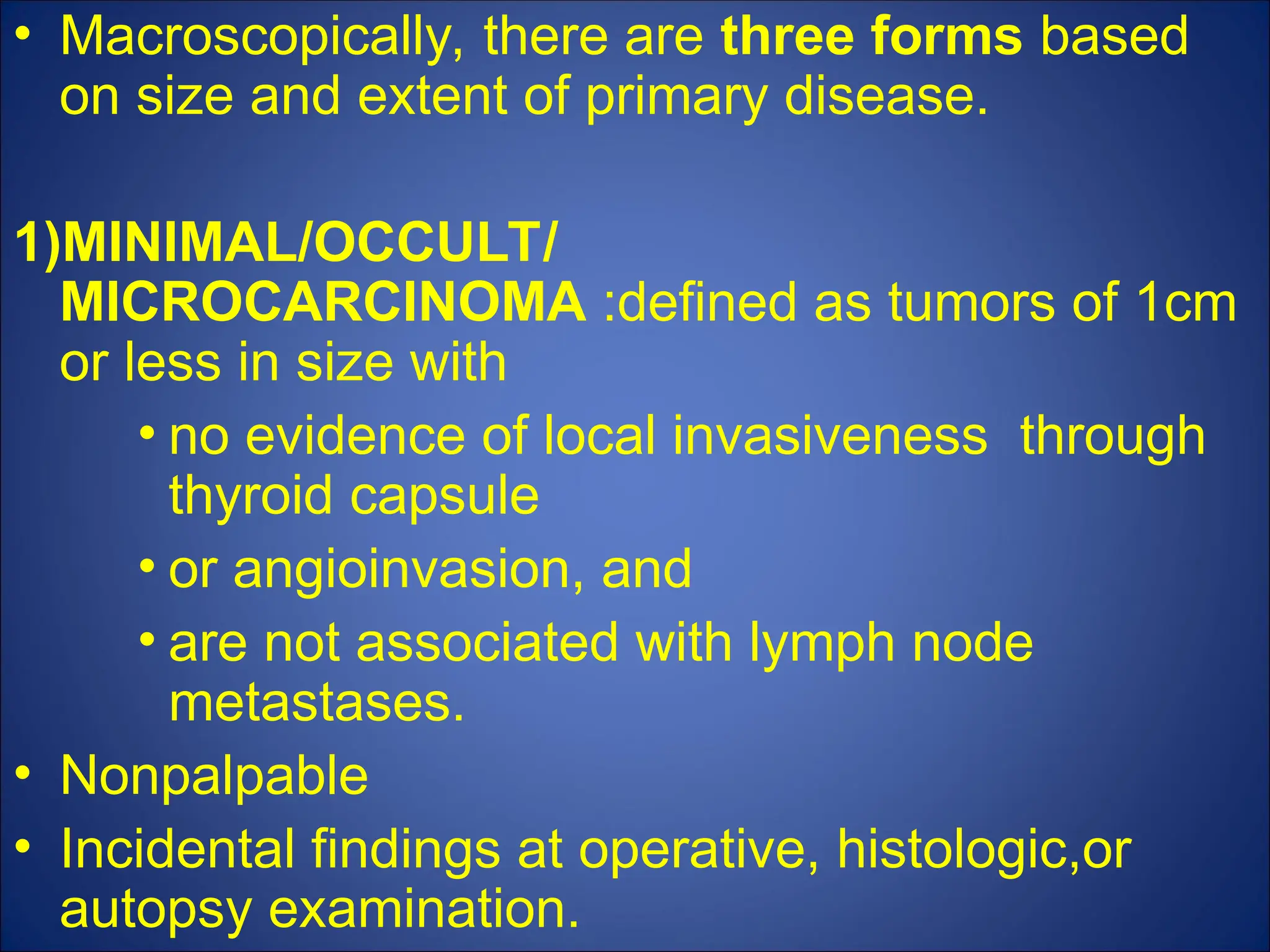
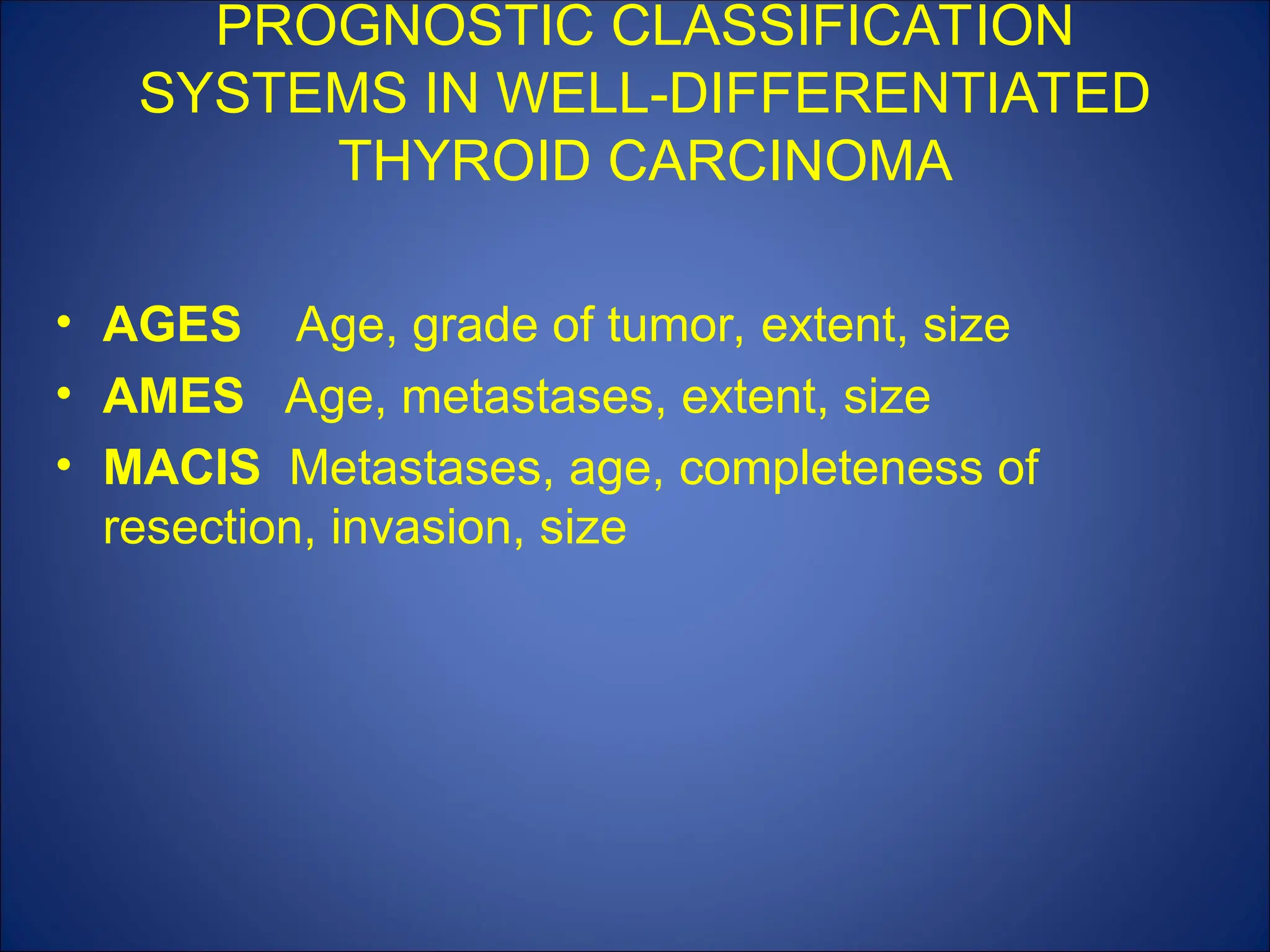
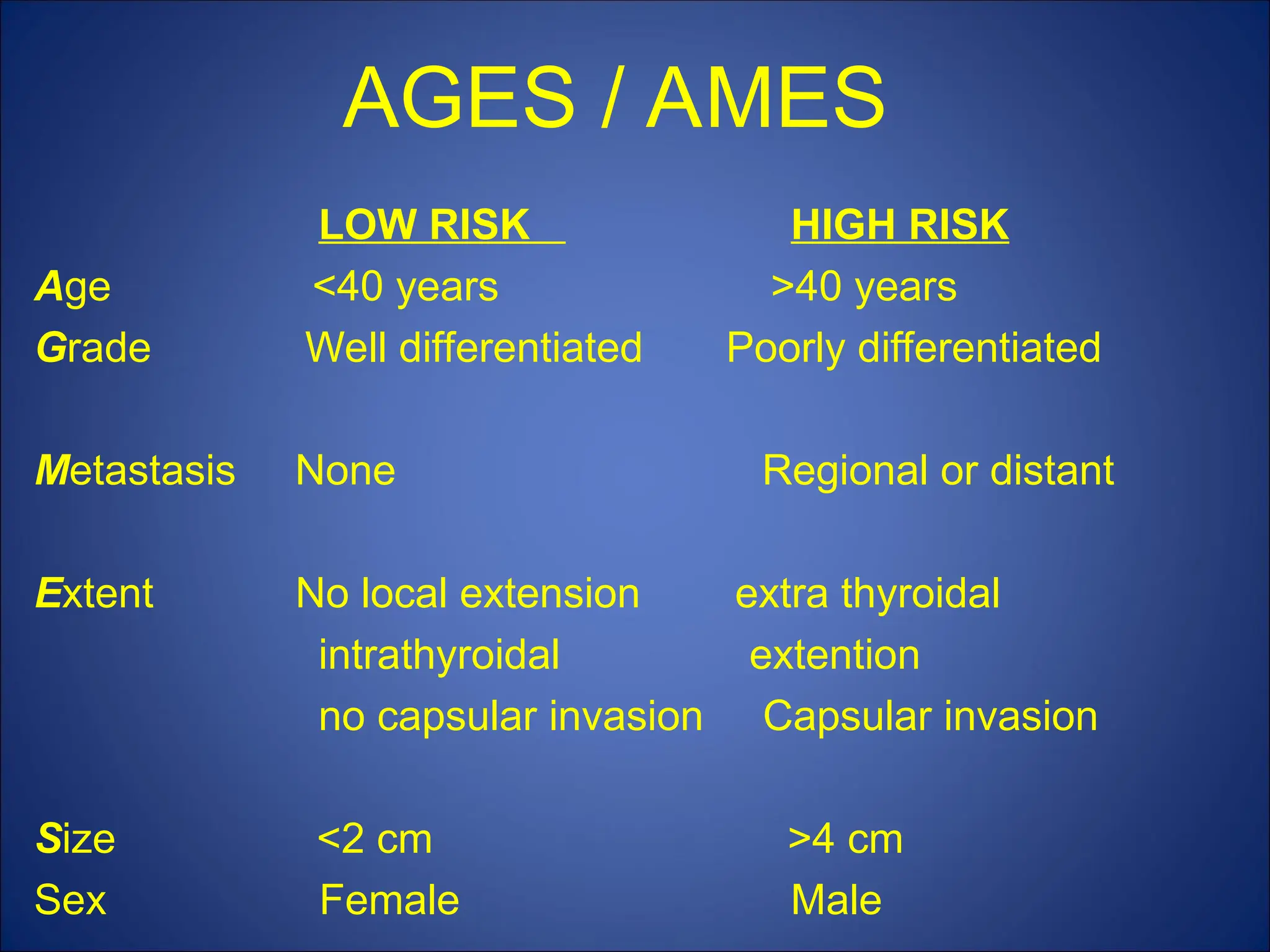
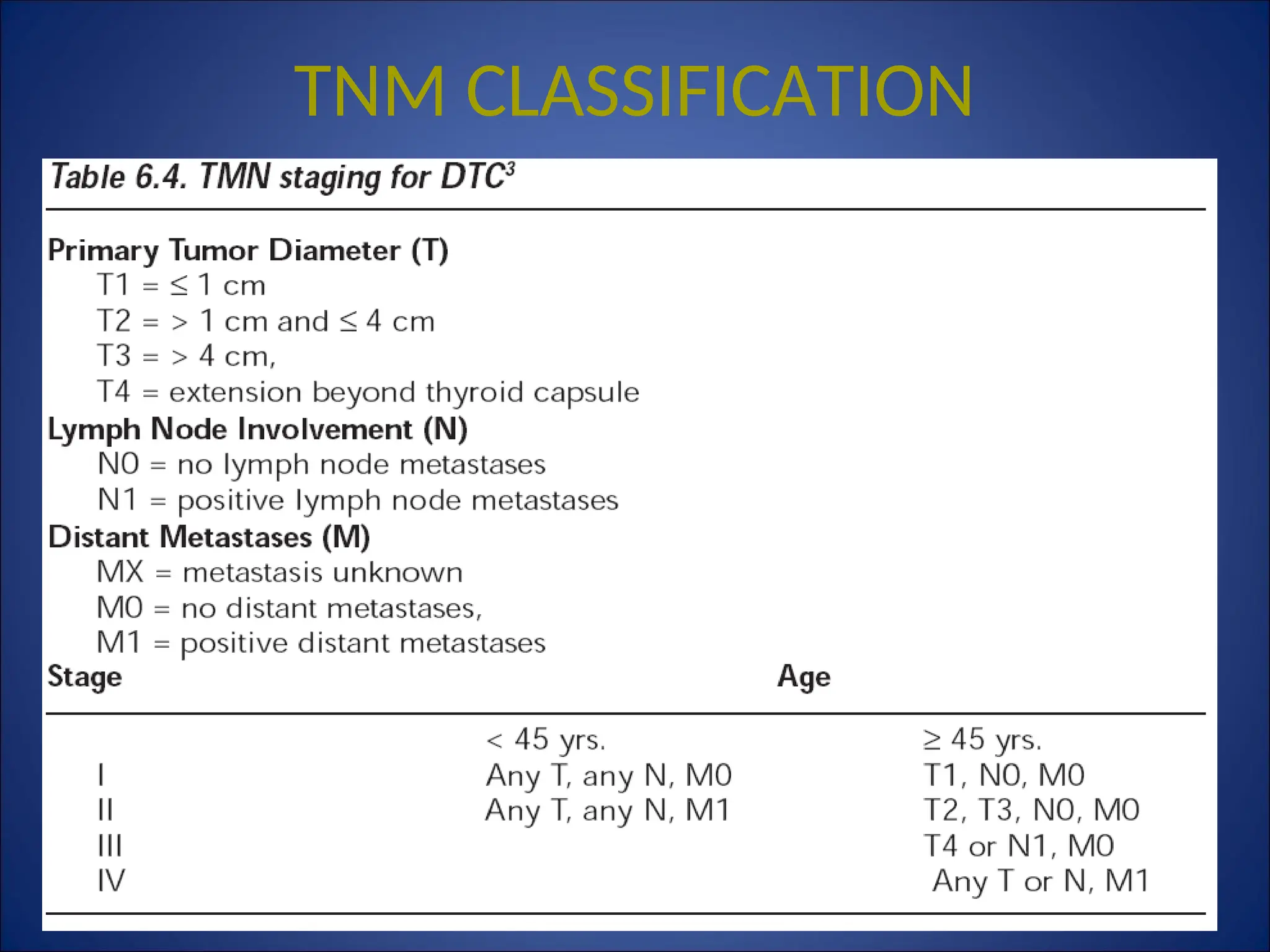
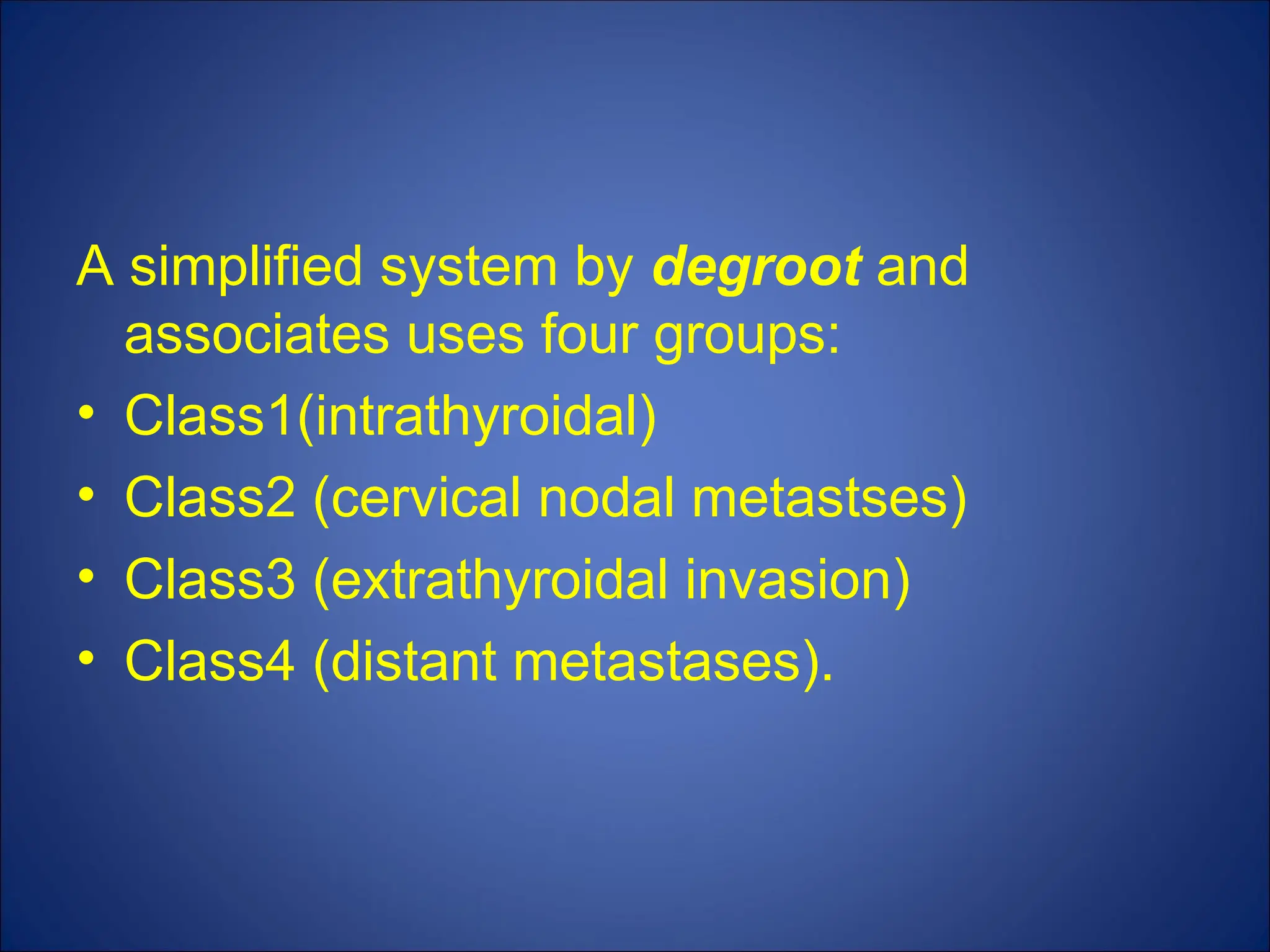
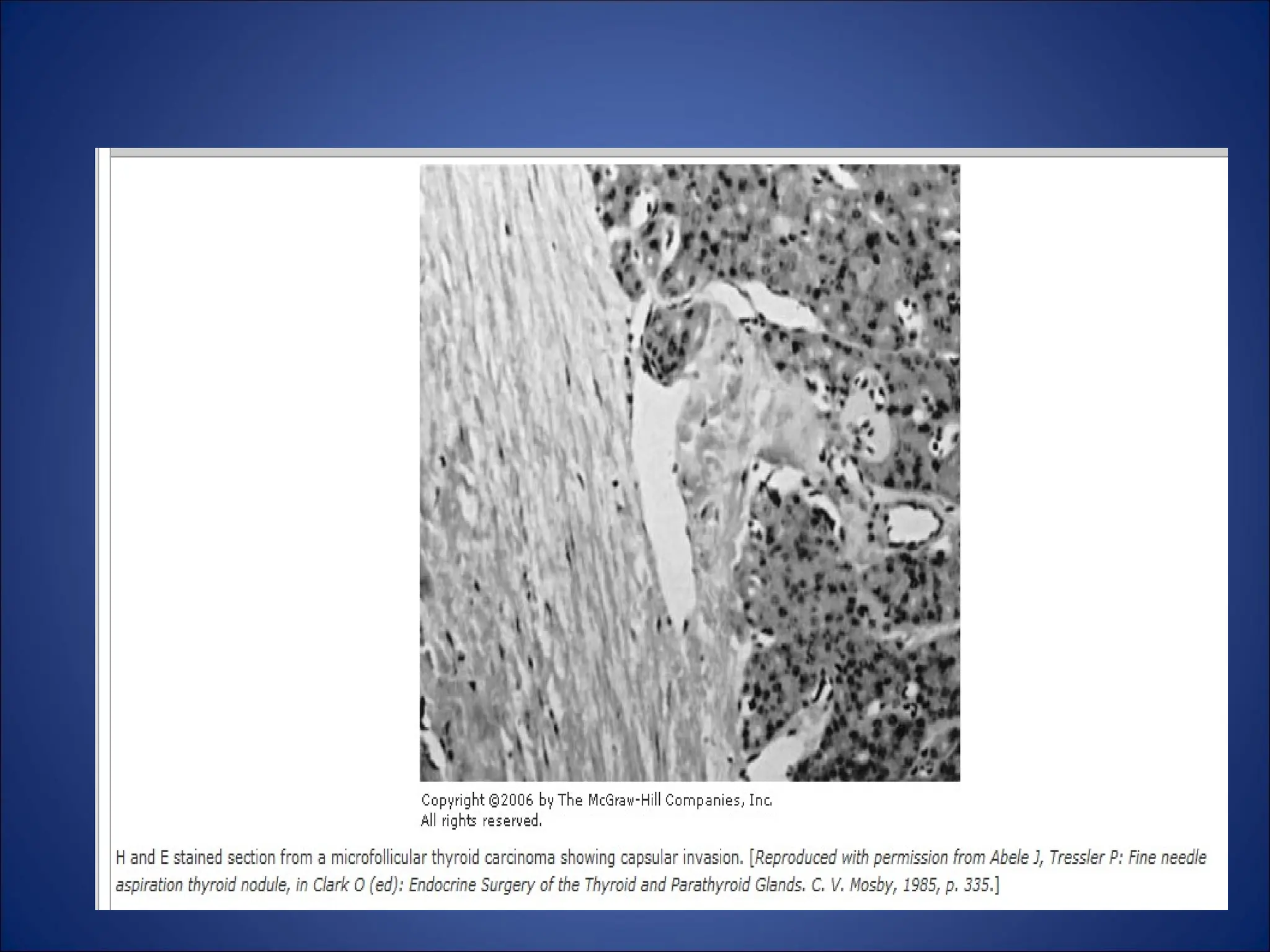
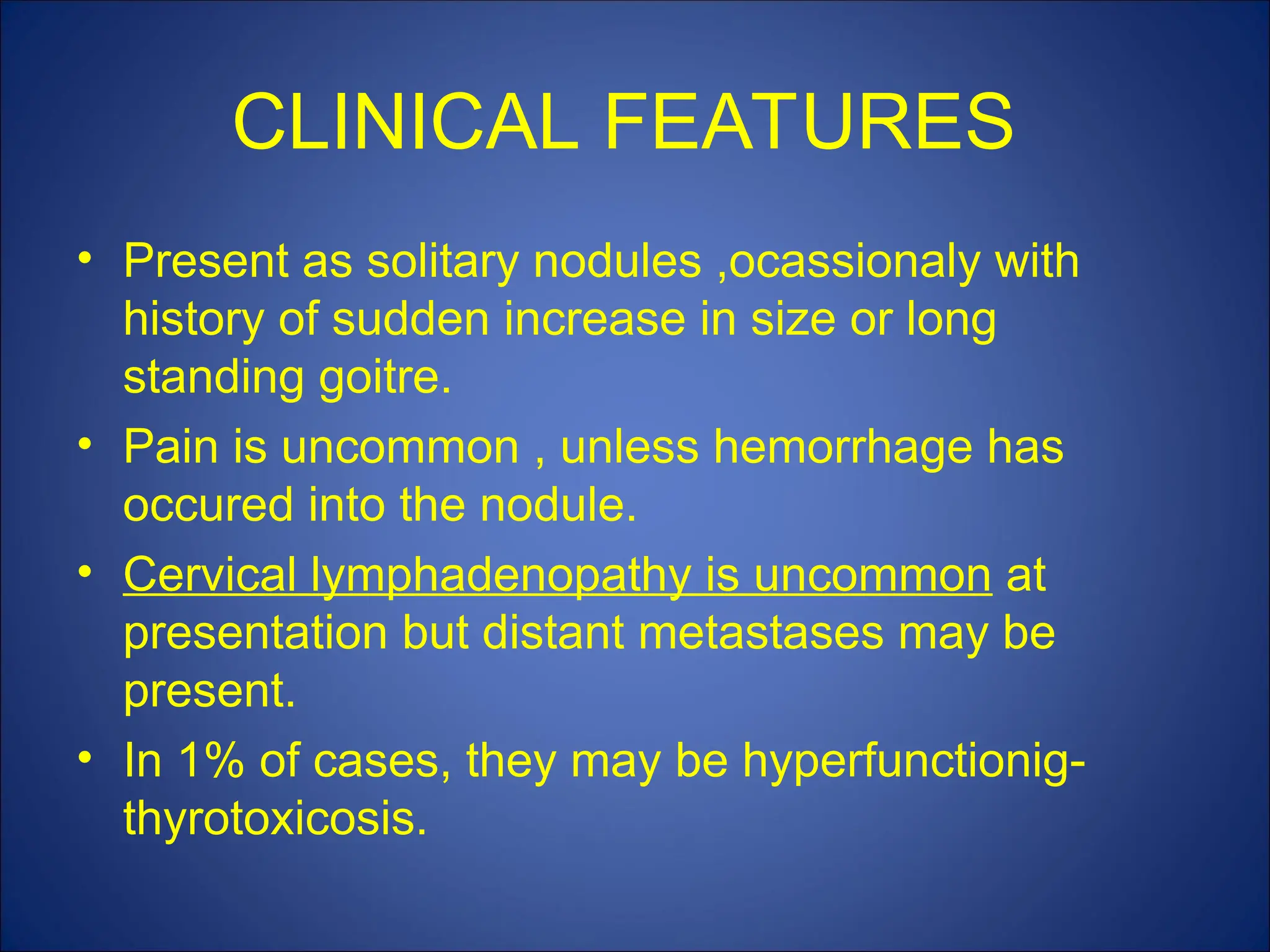
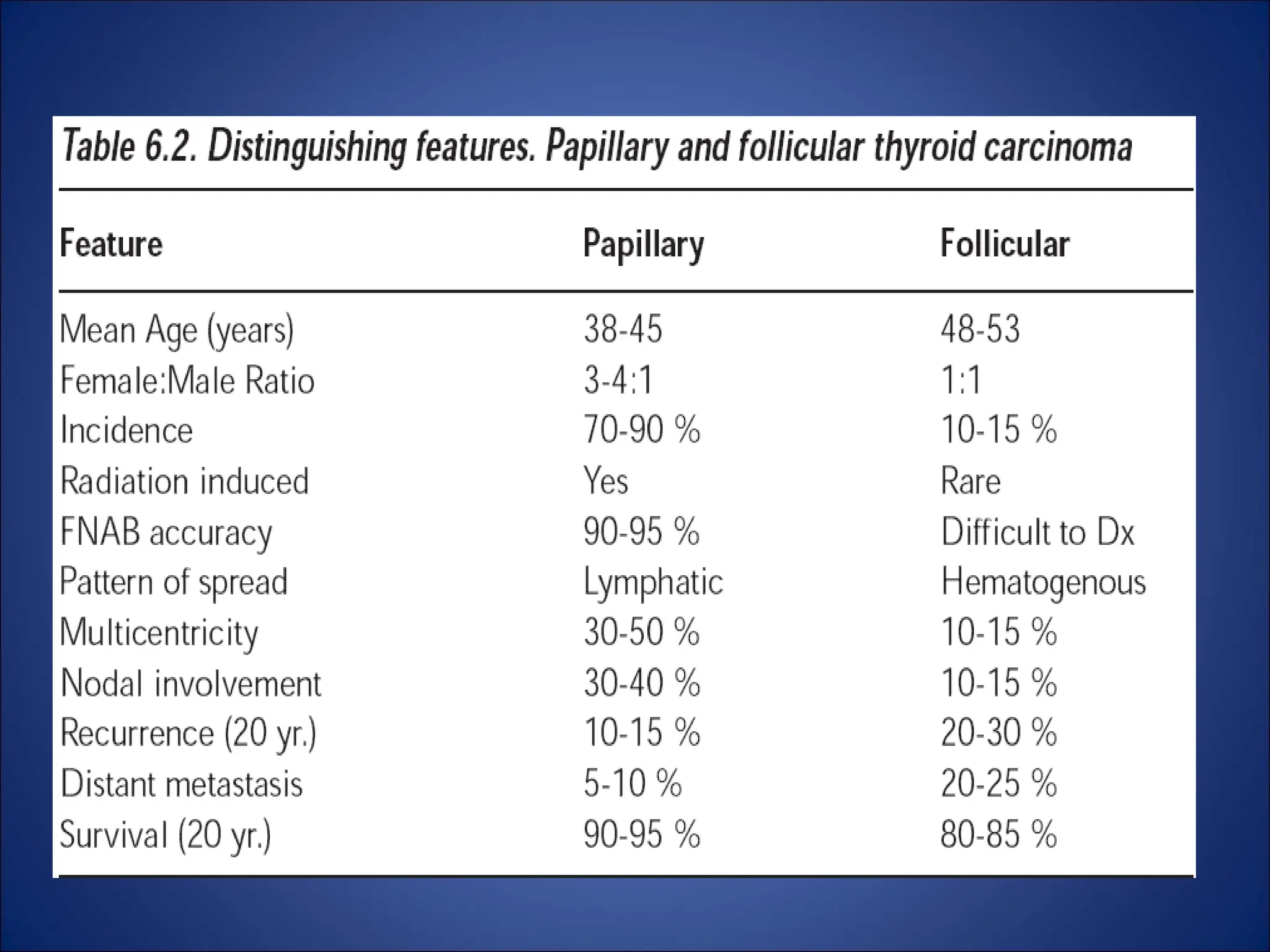
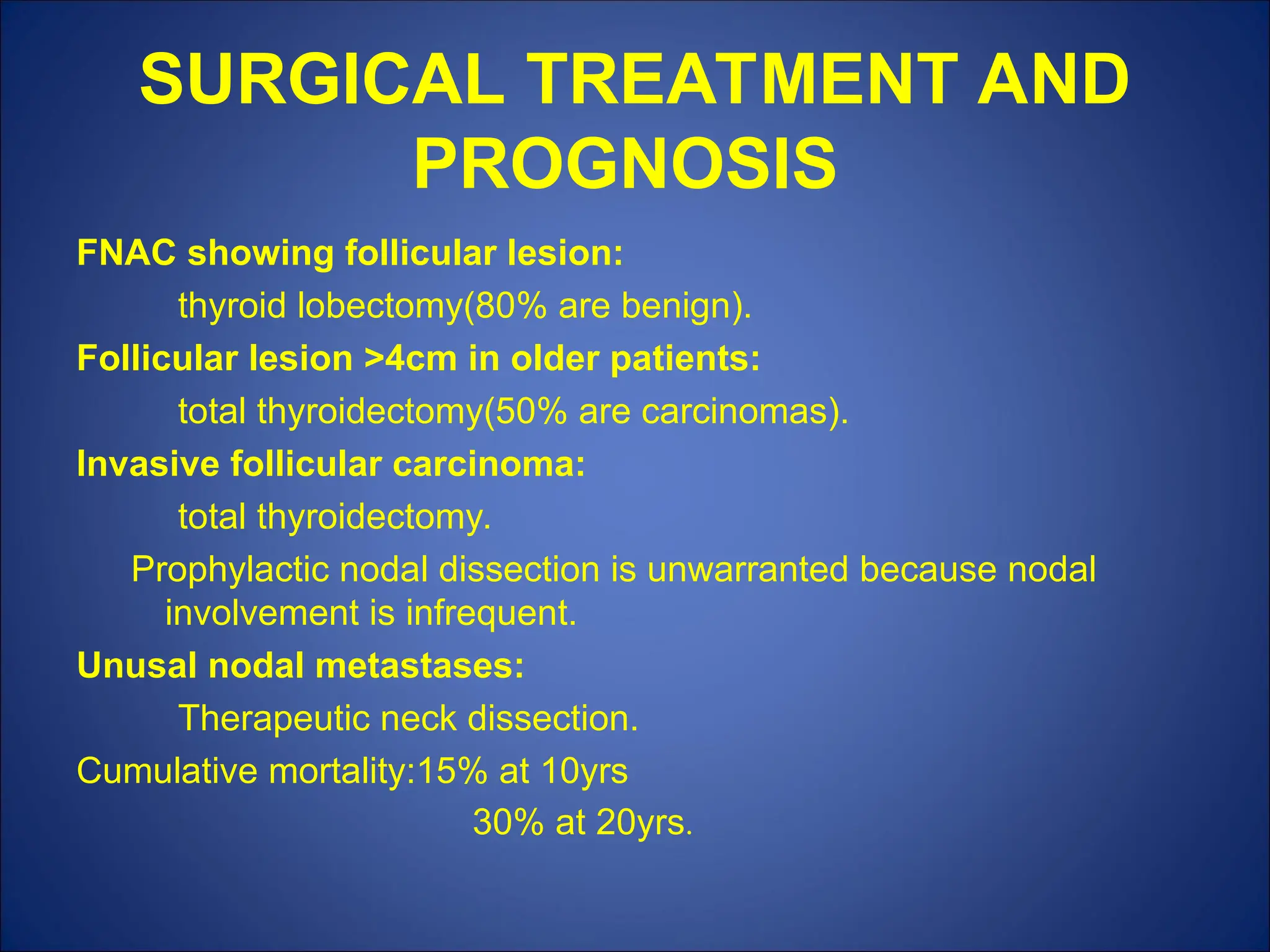
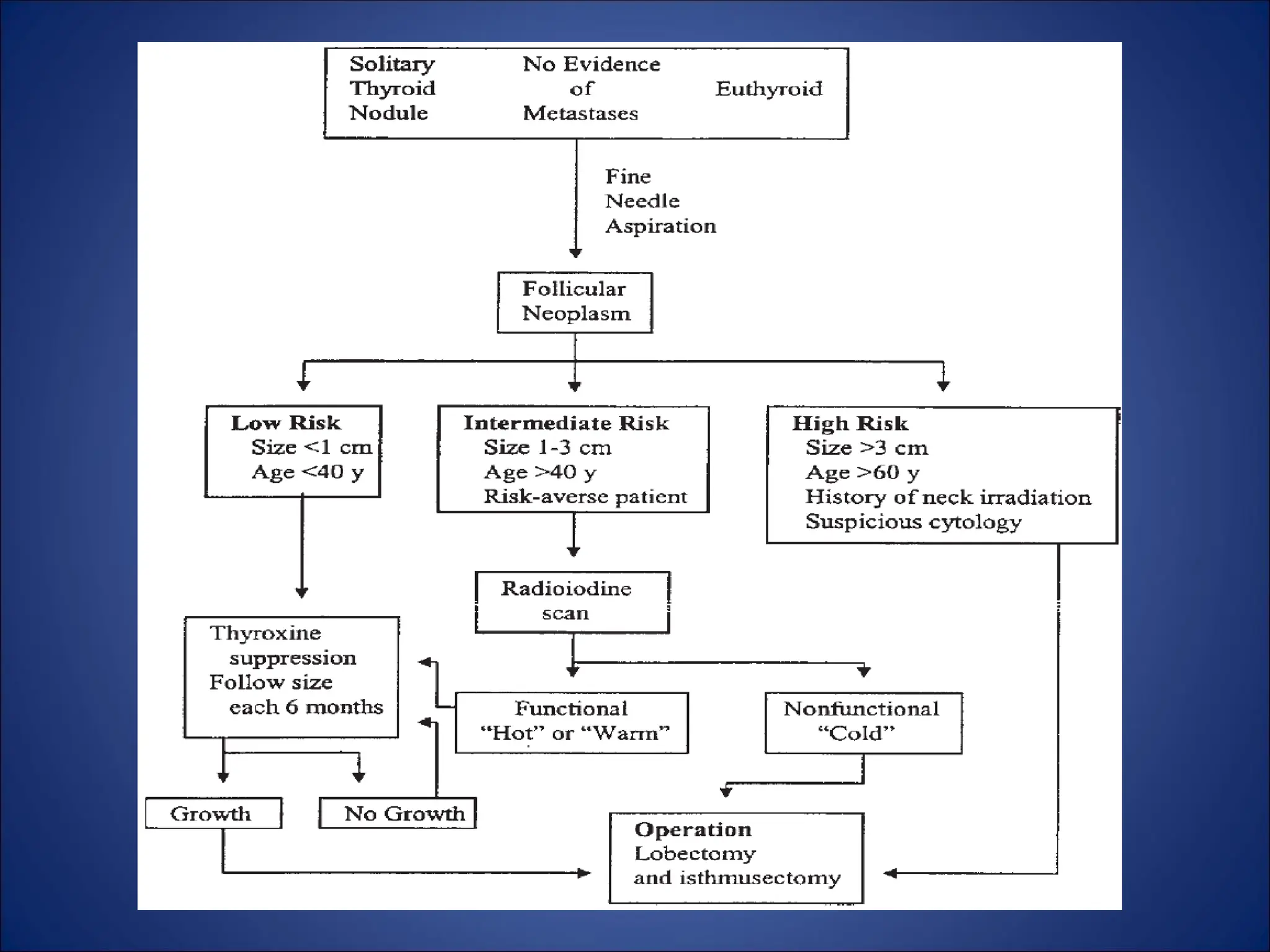
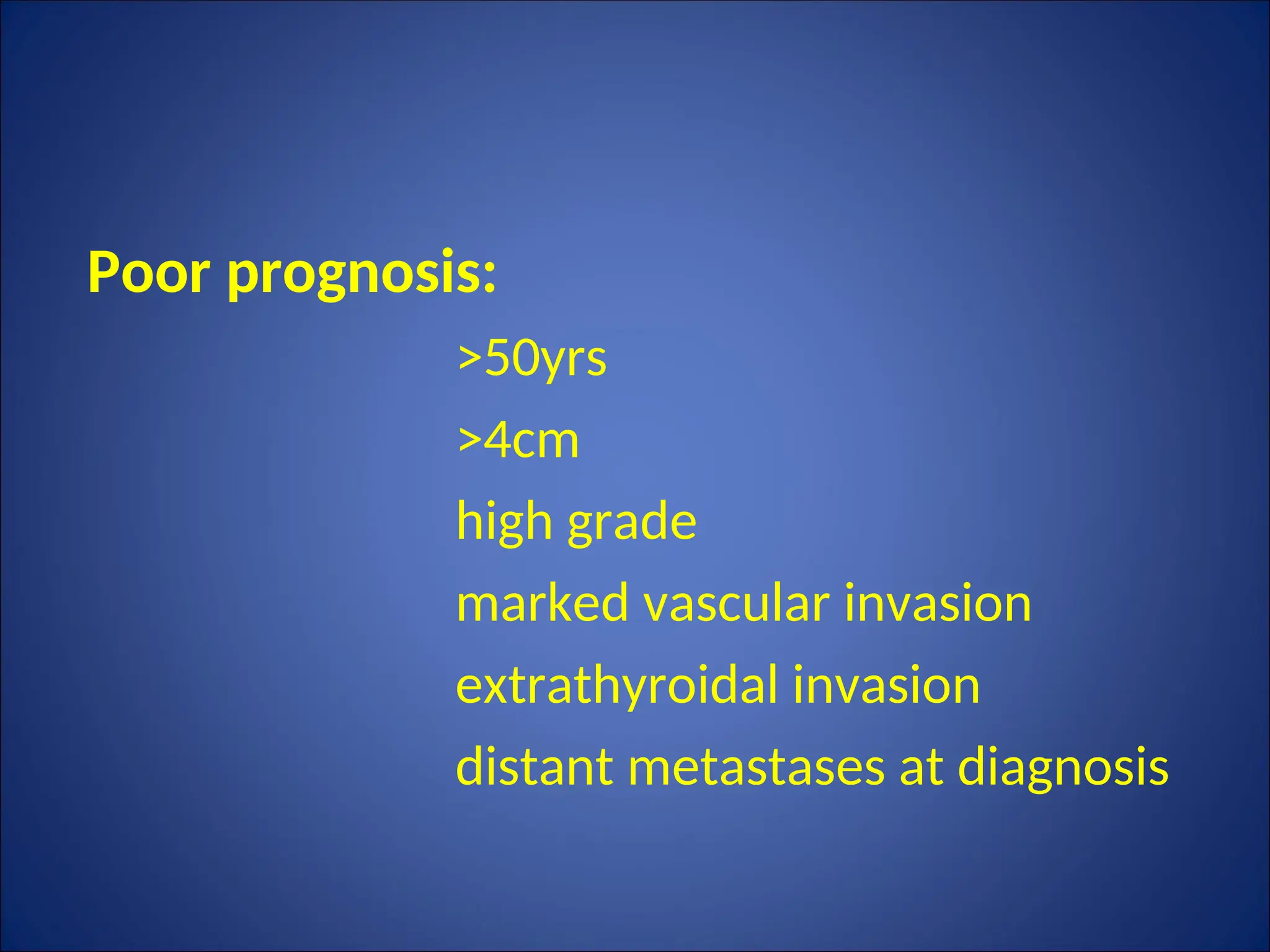
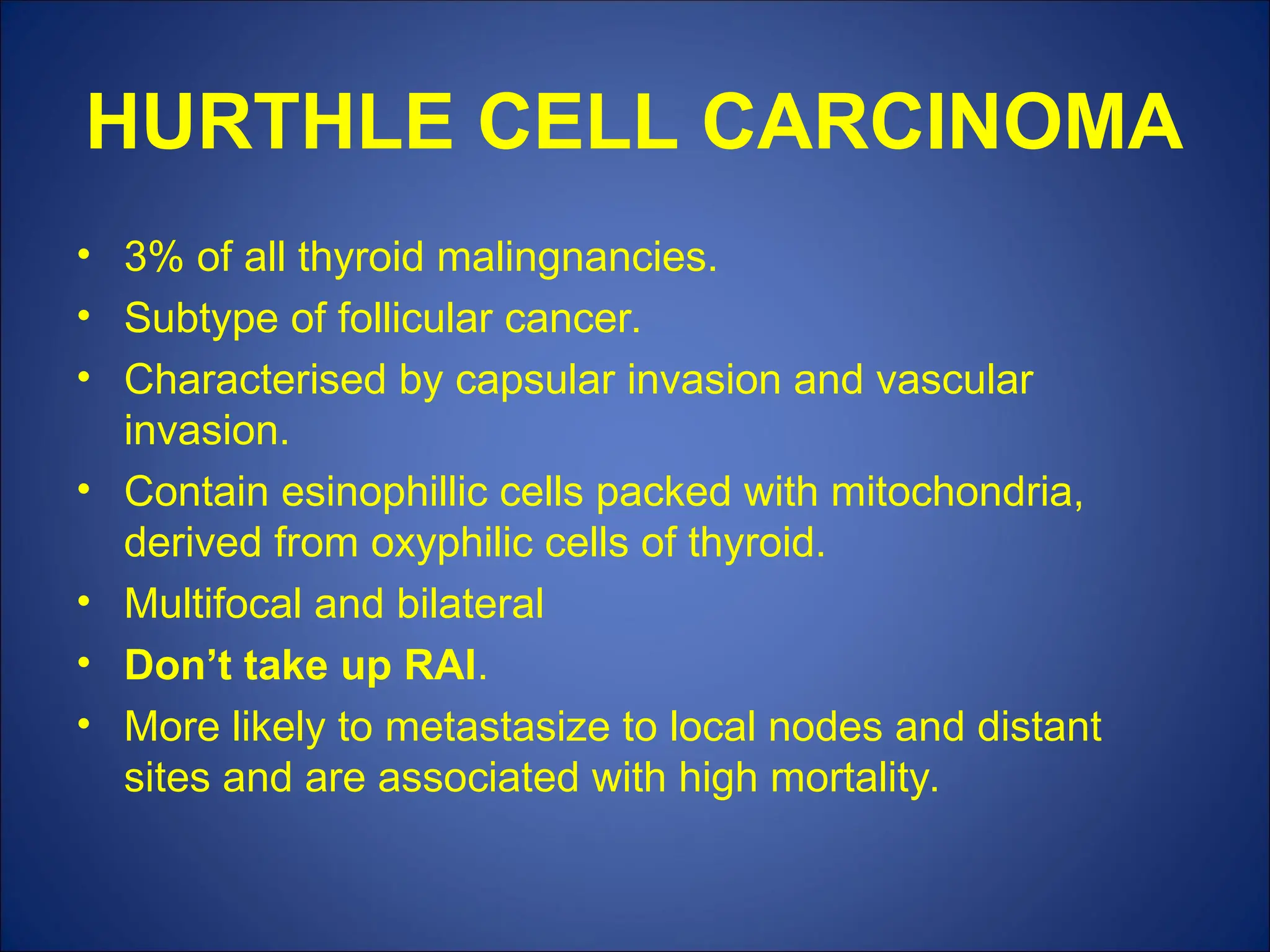
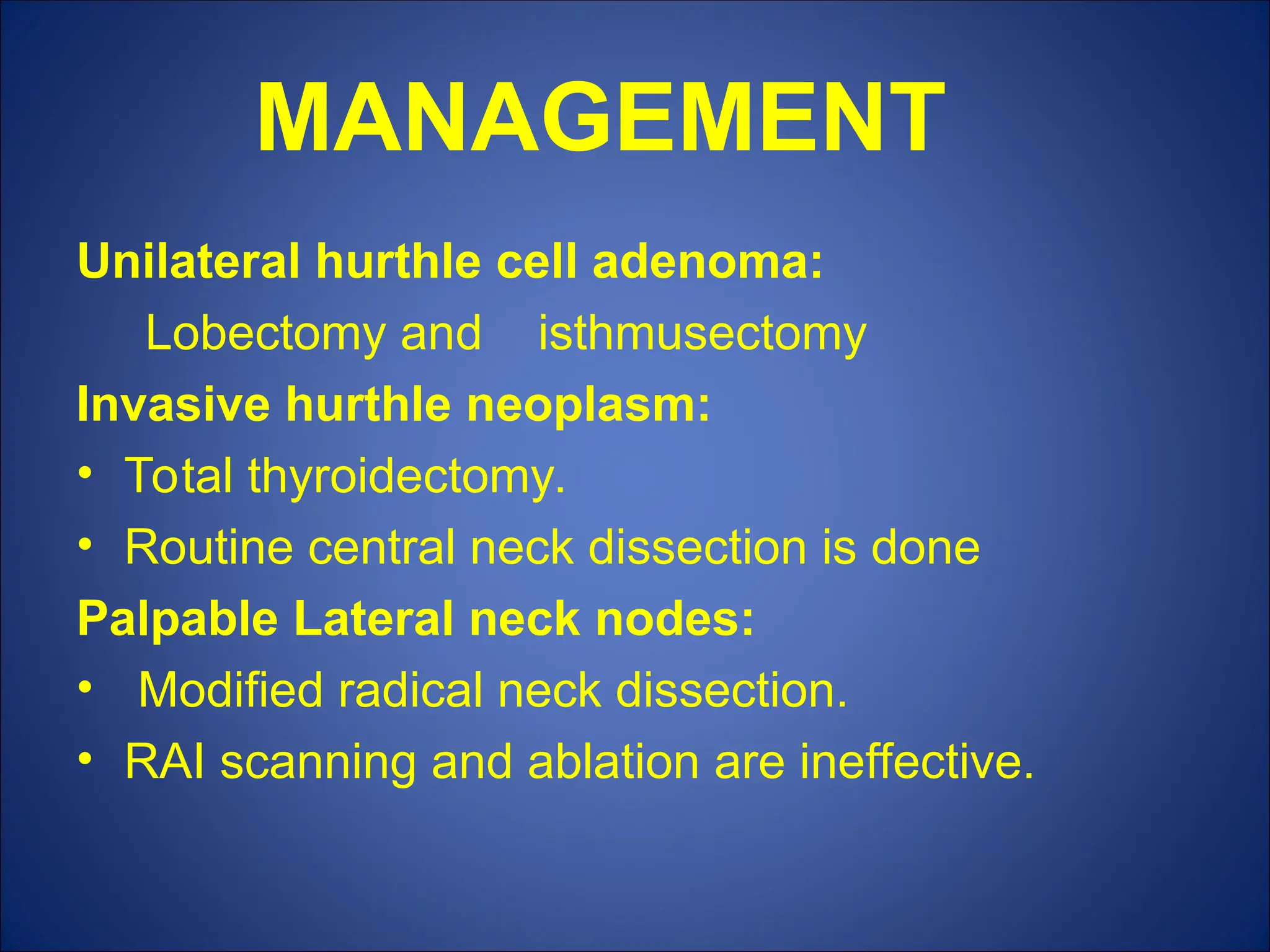
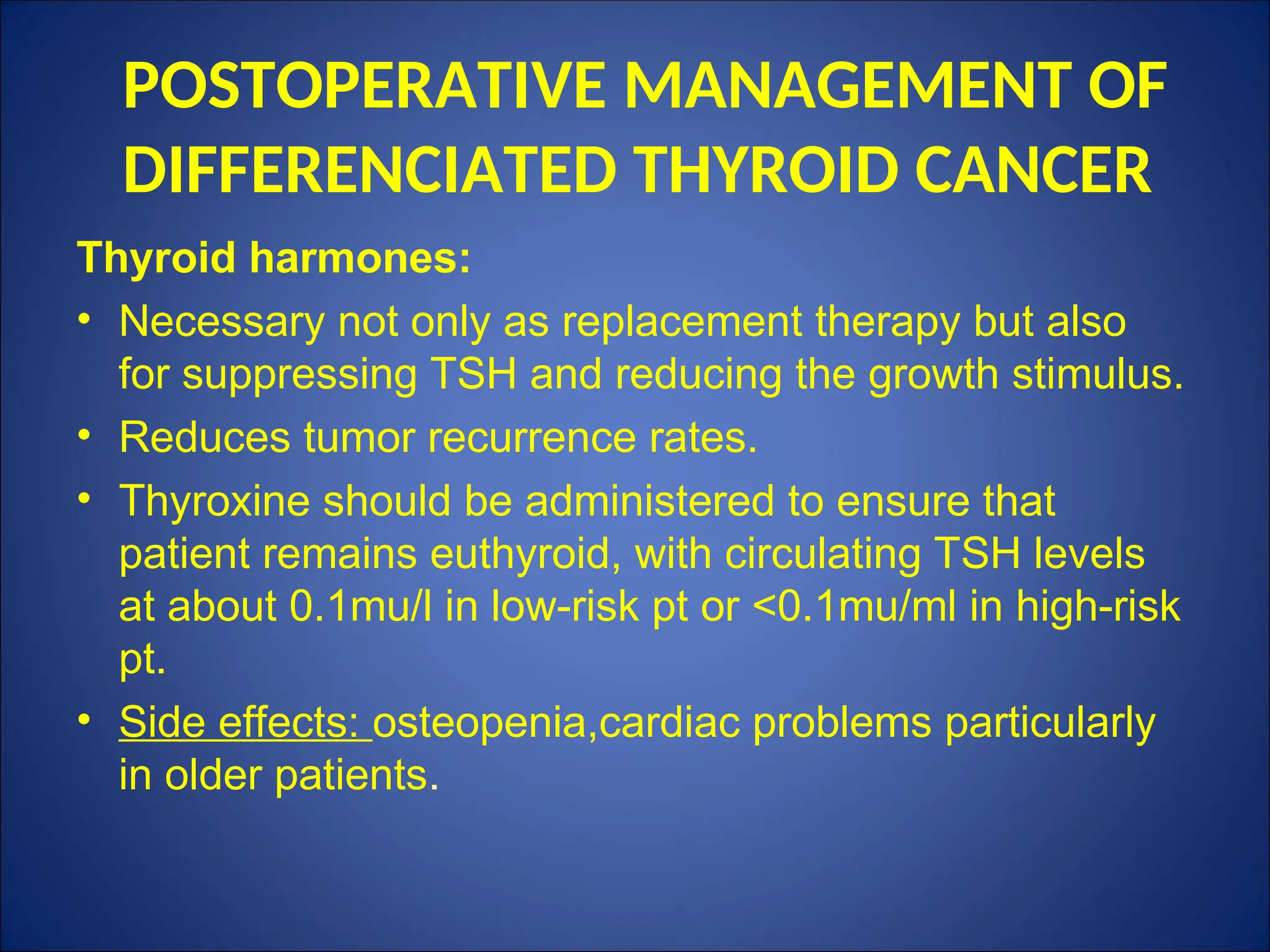
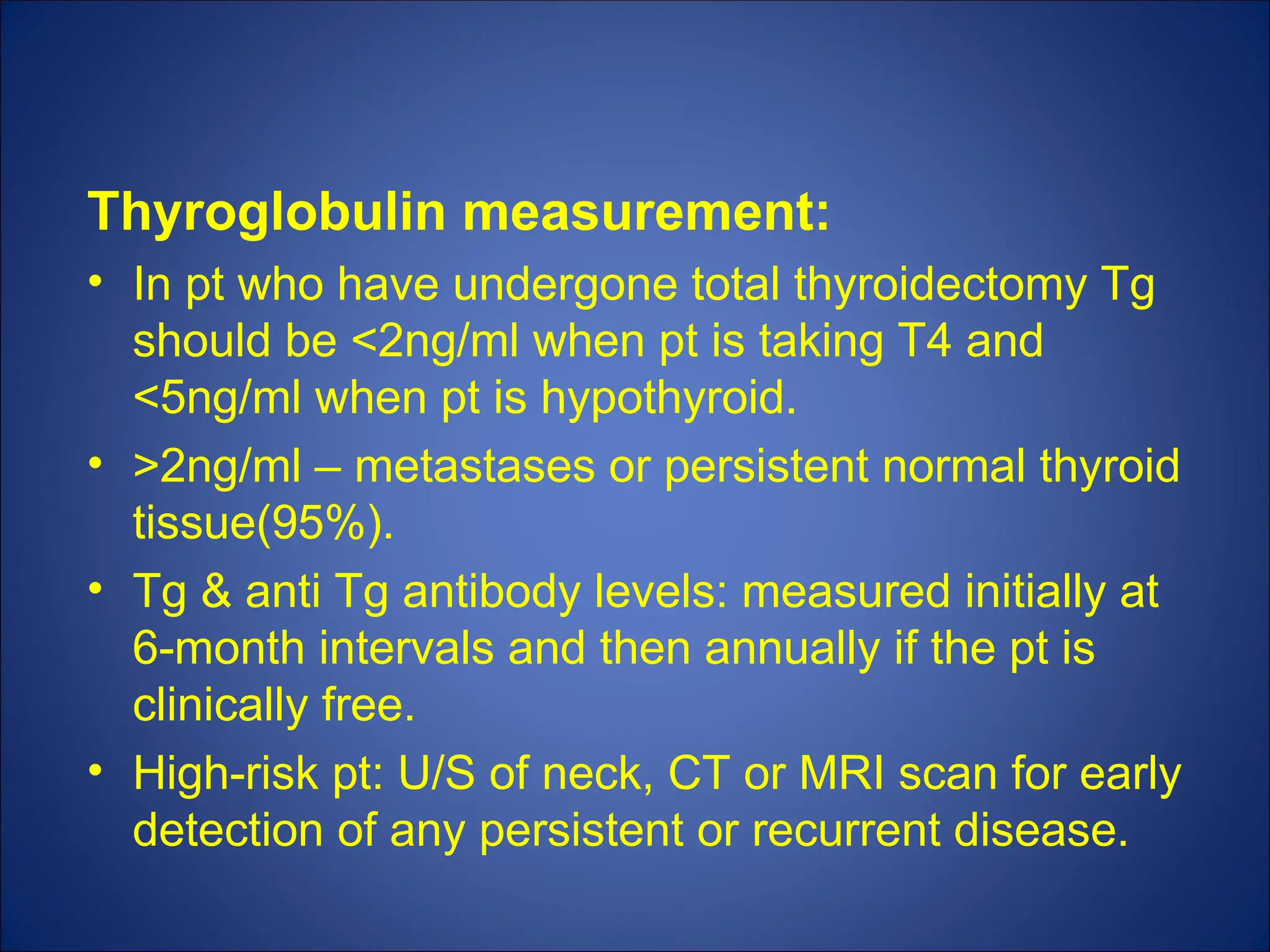
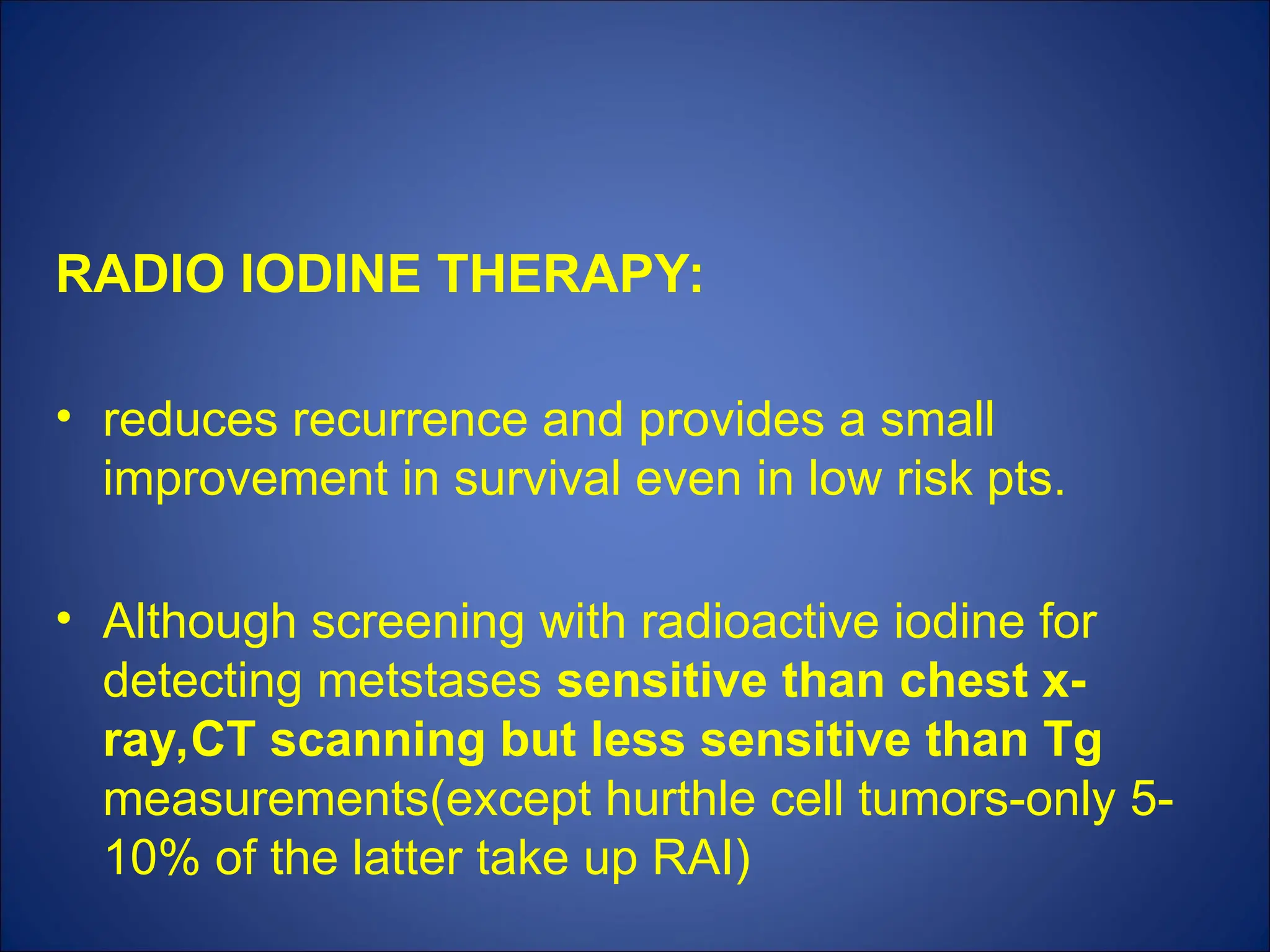
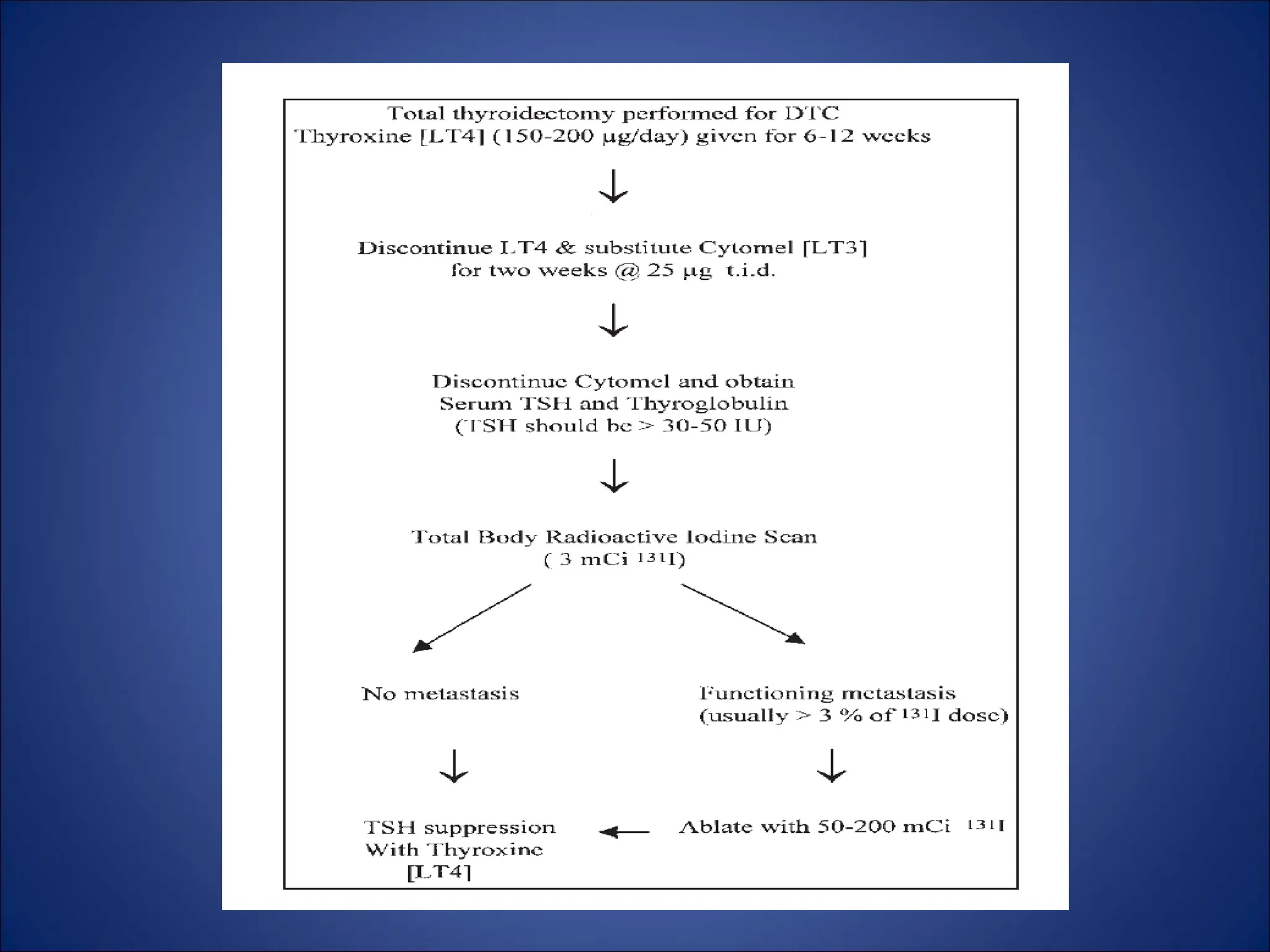
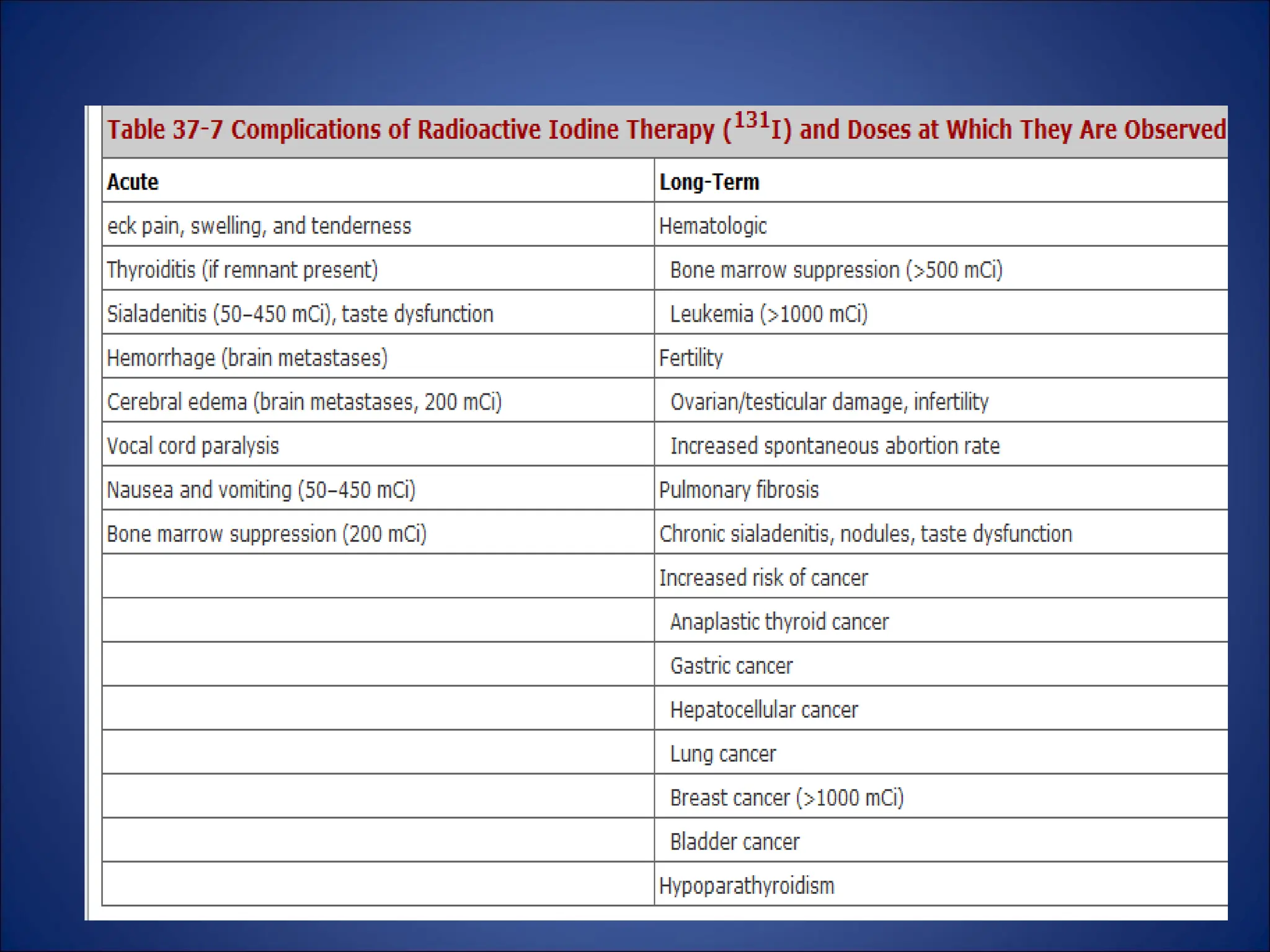
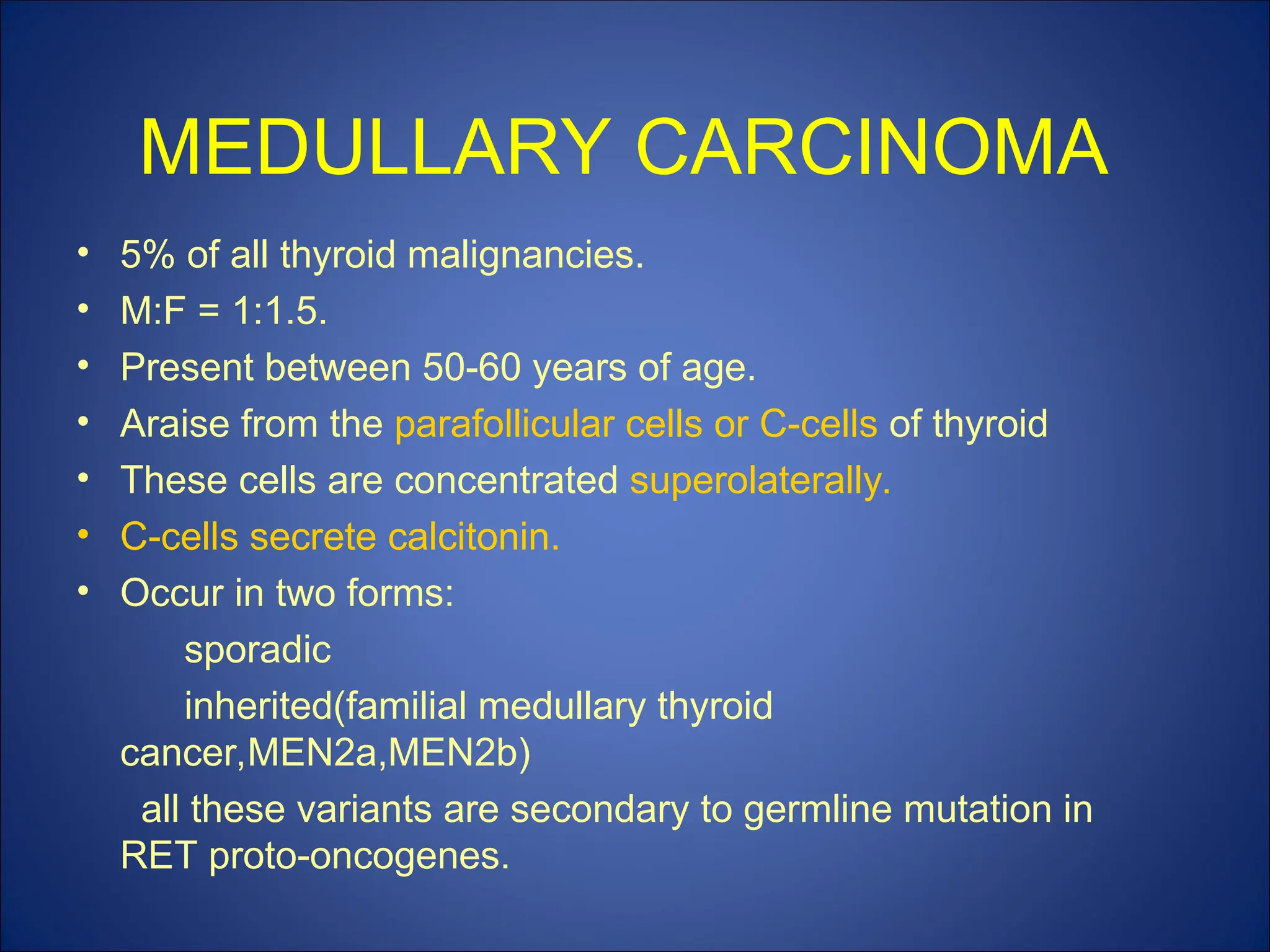
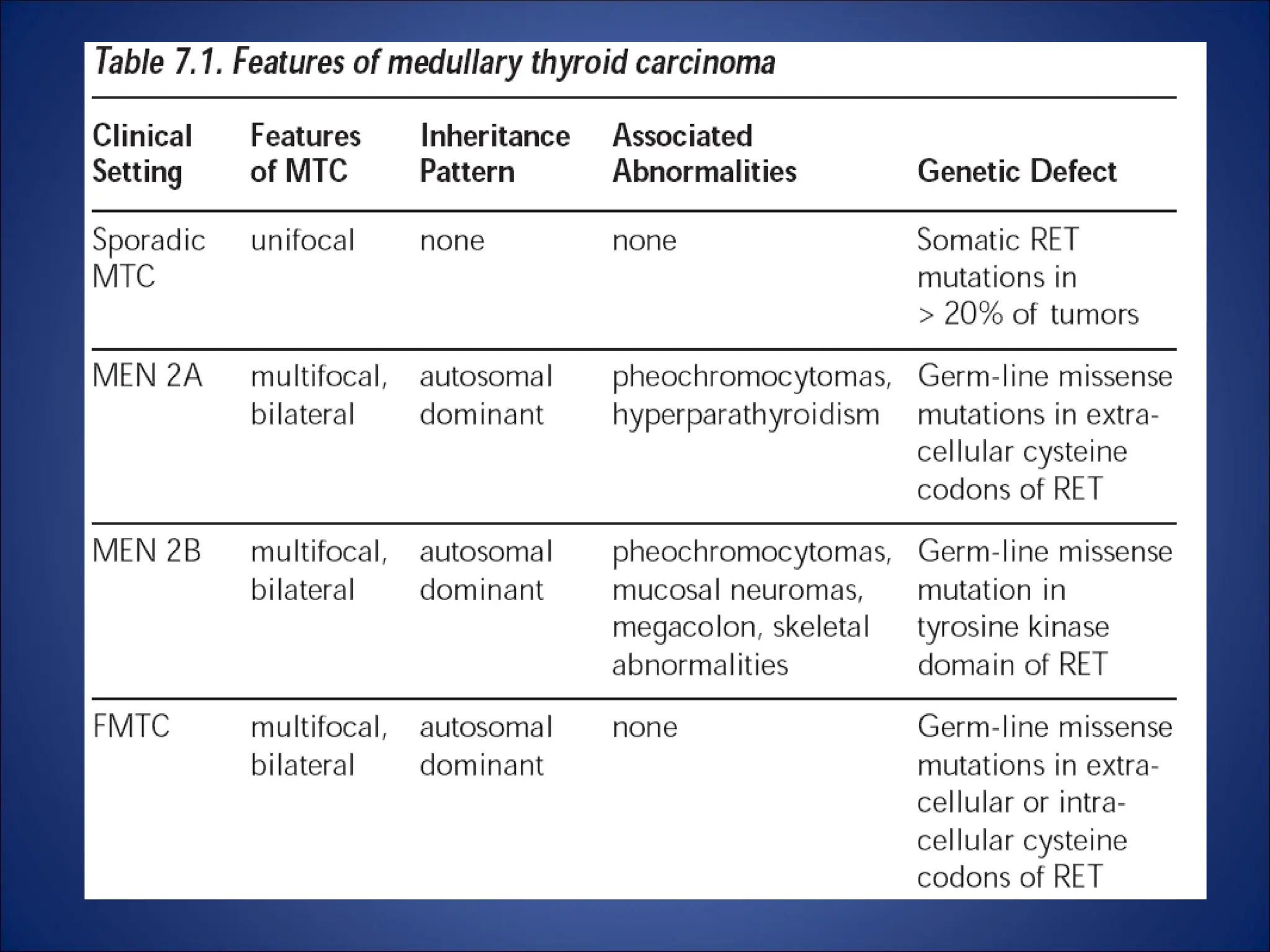
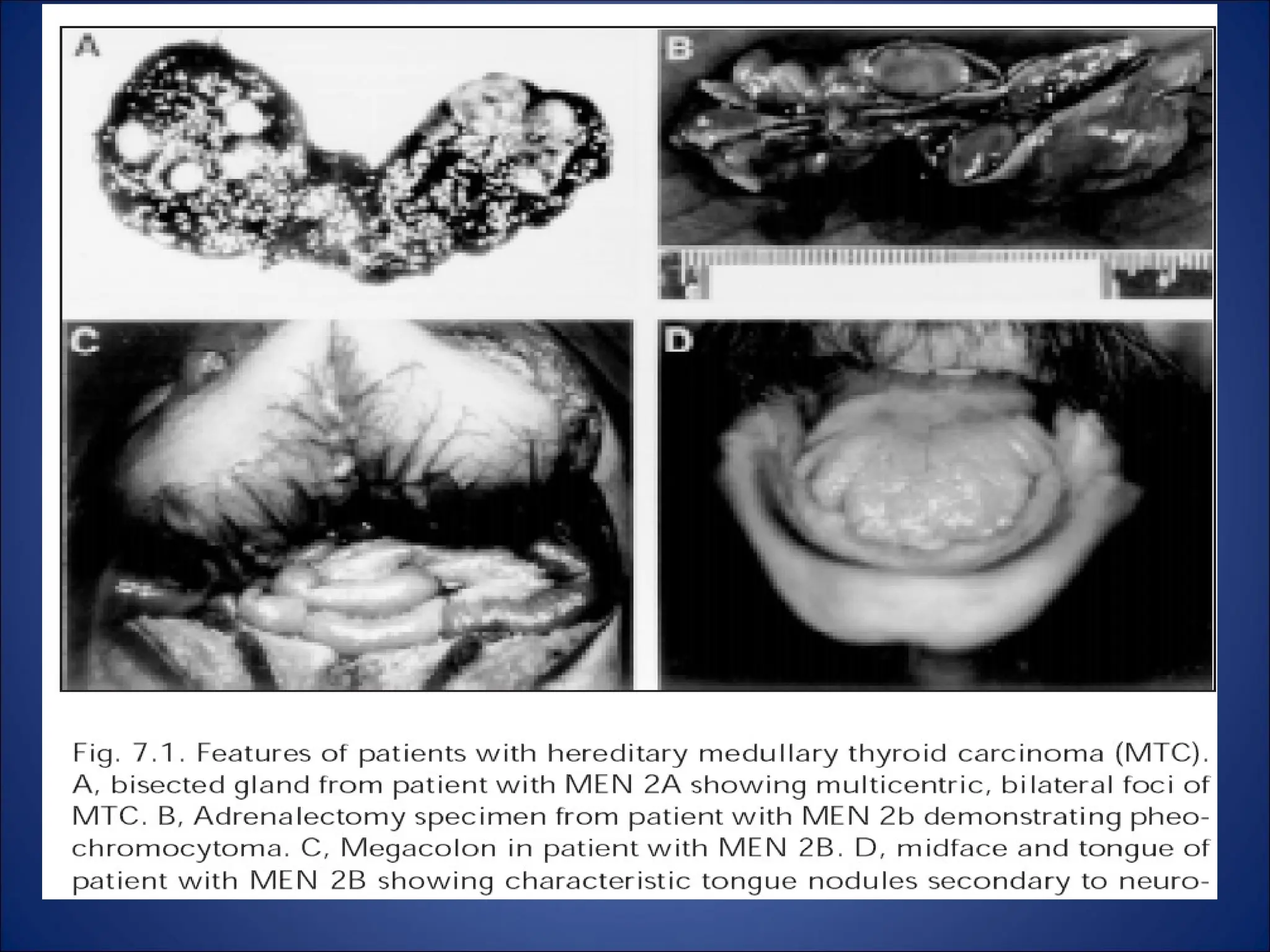
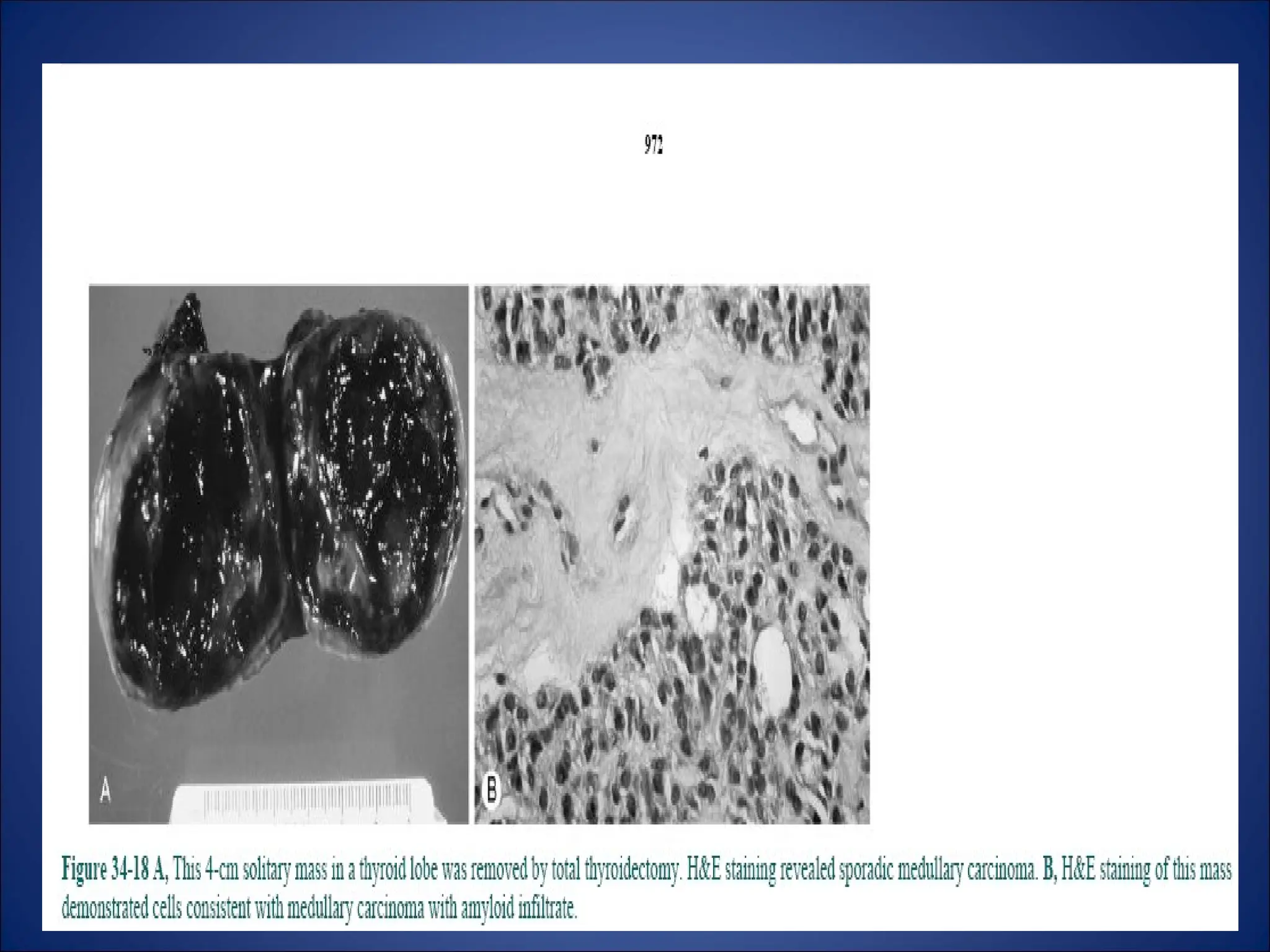
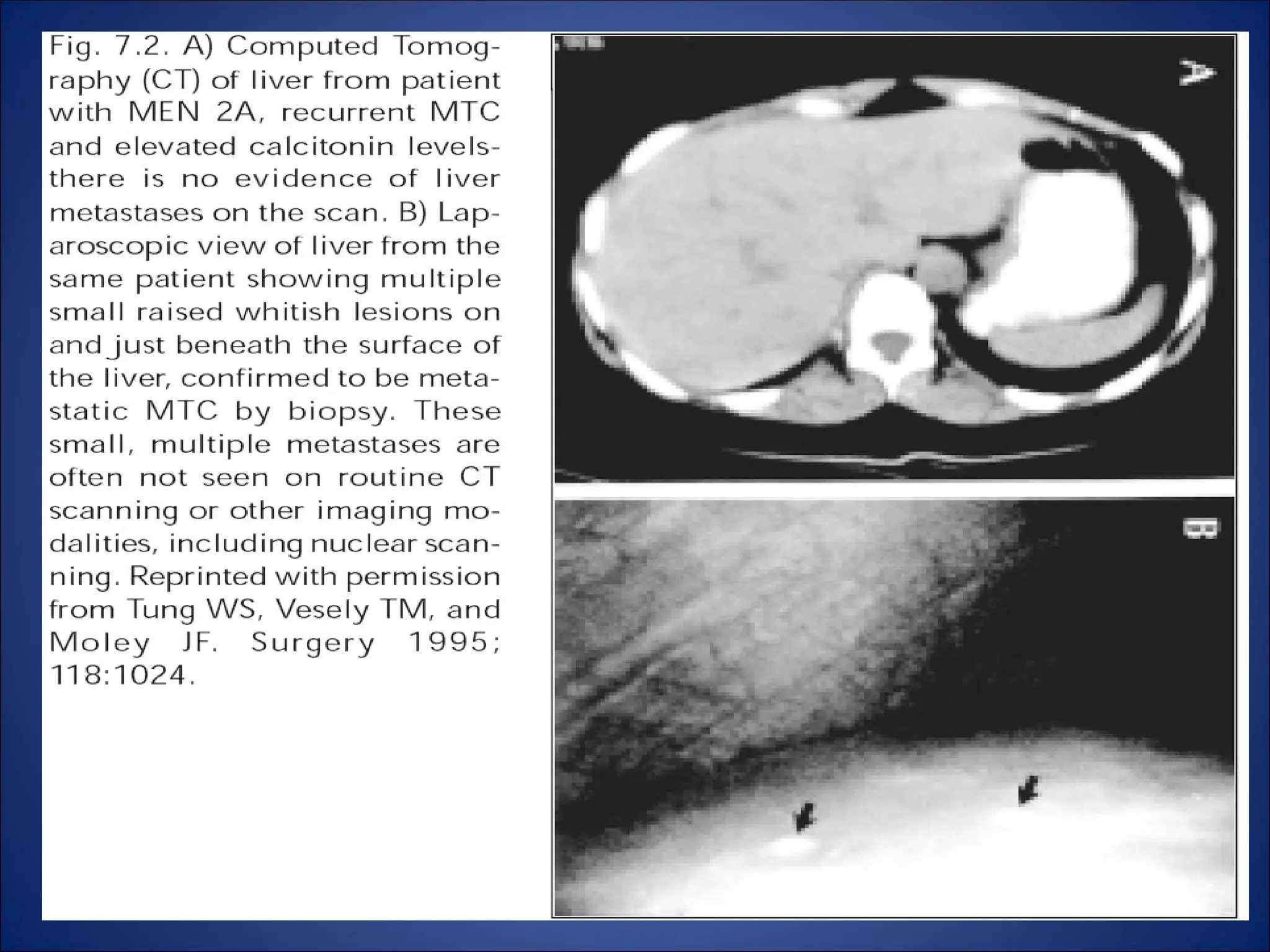
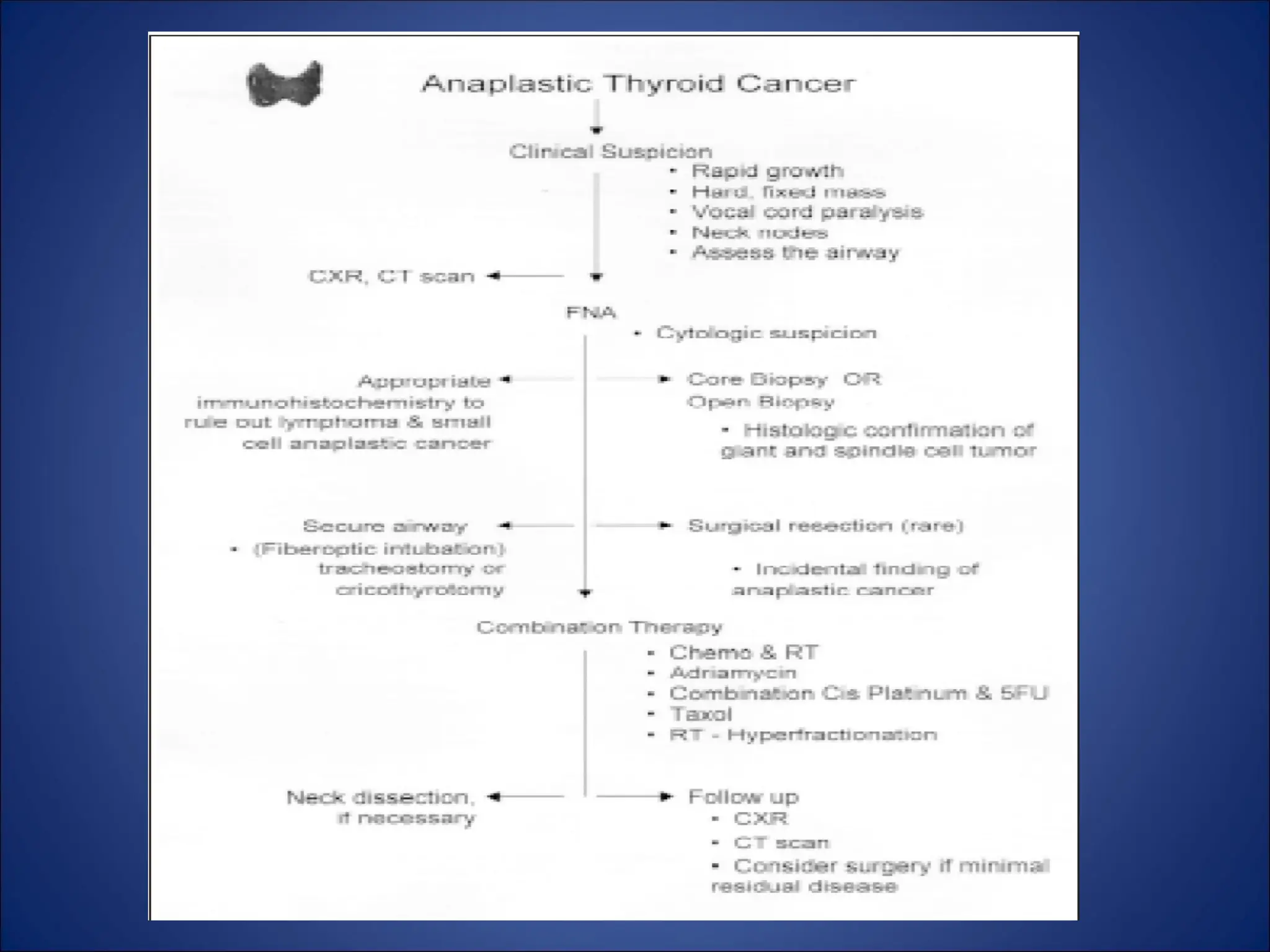
The document provides a comprehensive overview of thyroid neoplasms, discussing their classification into benign and malignant types, with detailed statistics on incidence rates. It highlights the different forms of thyroid cancer, such as papillary, follicular, medullary, and anaplastic carcinomas, along with their clinical features, diagnosis, and treatment options. Additionally, the document addresses prognostic factors, the role of surgical and medical management, and the implications of various genetic markers influencing outcomes.